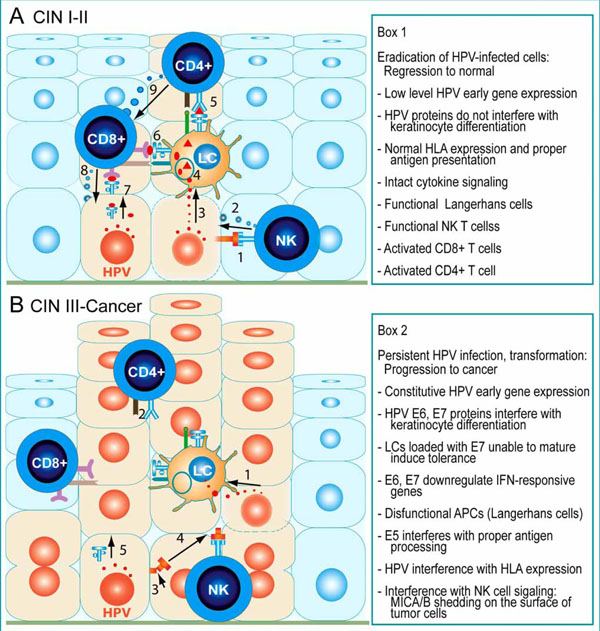
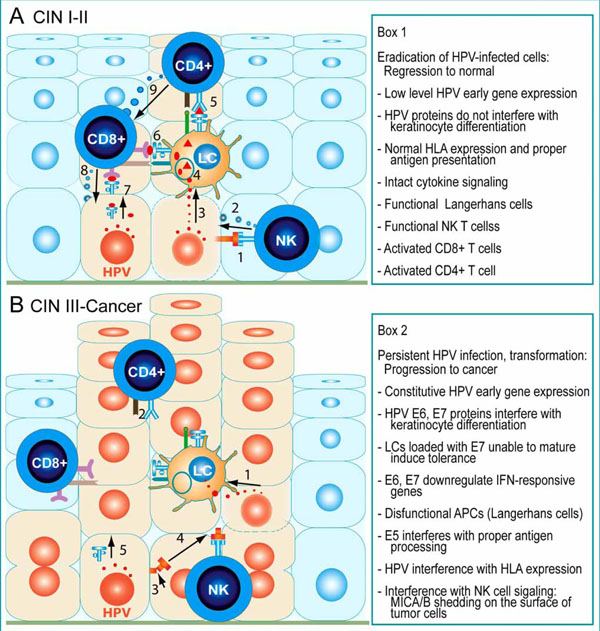
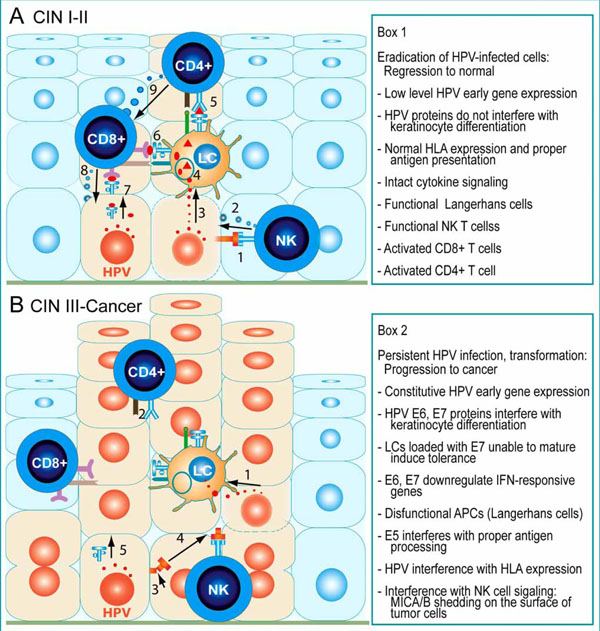
Fig. (3) Schematic representation of the cellular immune responses to keratinocytes infected by HR-HPVs in pre-cancer and cancer lesions of the uterine cervix. A, CIN I and II pre-cancer lesions usually regress spontaneously as result of effective innate and adaptive cytotoxic responses. Intraepithelial NK cells become activated by ligands of the NKG2D receptor (1), such as the MHC class I-related molecules A and B (MICA and MICB), expressed on the surface of HPV-infected cells, and release the contents of cytolytic granules (2) on the target cell. LCs are intraepithelial professional presenting cells, which take up viral antigens (3) released by apoptotic HPV-infected cells, and subsequently present viral epitopes (4) to CD4+ (5) and CD8+ T cells (6), which become activated. Upon recognition of HPV antigens presented by MHC class I molecules on the surface of HPV-infected cells (7), activated CD8+ T cells also release cytolytic granules (8). These granules contain serine proteases called granzymes, which induce programmed cell death in the target cells. Activated CD4+ T cells secrete cytokines that stimulate cytolytic CD8+ T cells (9). Box 1 summarizes the conditions that allow recognition and eradication of HPVinfected cells by the immune cells. B, Advanced cervical CIN III pre-cancer and cancer lesions progress while the effectors of cellular immunity remain passive or unable to eliminate the HPV-infected/transformed cells. LCs loaded with HPV antigens (1) released by HPVinfected cells are unable to mature and cannot present antigen to and activate CD4+ and CD8+ T cells. Instead, CD4+FoxP3+ regulatory T cells infiltrate the lesion and down-regulate effector T lymphocytes. Further, NKG2D-ligands on the surface of infected cells undergo cleavage and their ectodomains are released (2) as soluble molecules that bind NKG2D on NK cells (3), which thereby become inactive (4). In addition, antigen presentation is altered (5). The mechanisms used by HPV to evade immunosurveillance are listed in Box 2.