- Home
- About Journals
-
Information for Authors/ReviewersEditorial Policies
Publication Fee
Publication Cycle - Process Flowchart
Online Manuscript Submission and Tracking System
Publishing Ethics and Rectitude
Authorship
Author Benefits
Reviewer Guidelines
Guest Editor Guidelines
Peer Review Workflow
Quick Track Option
Copyediting Services
Bentham Open Membership
Bentham Open Advisory Board
Archiving Policies
Fabricating and Stating False Information
Post Publication Discussions and Corrections
Editorial Management
Advertise With Us
Funding Agencies
Rate List
Kudos
General FAQs
Special Fee Waivers and Discounts
- Contact
- Help
- About Us
- Search

The Open Clinical Cancer Journal
(Discontinued)
ISSN: 1874-1894 ― Volume 5, 2011
The Changing Management of Esophageal Carcinoma: Survival in a Population Cohort 1985-1994
T. Bates1, *, A. Antoniou2, R.E.K. Marshall3, M. Harrison1 , E.E. Bassett4
Abstract
Background:
The management of esophageal carcinoma is changing but before the introduction of chemotherapy and multidisciplinary teams, surgery became more selective. The aim of this study was to confirm this trend and to examine survival in a total population cohort 1985-94.
Results:
Only a quarter of 413 patients had surgery but from 1989 even fewer were operated on but there were more long-term survivors: 1/51 v. 7/58 (p<0.05). Operative mortality fell from 12% to 6.9 % in the later period (N.S.) and survival post surgery was marginally improved, 15 v. 11 months p = 0.0502. The five year survival rate doubled from 7.8% to 17.2%.
Conclusion:
Few studies of esophageal cancer include all cases in a defined population. This carries a very poor prognosis but the present cohort shows a slight improvement with more selective surgery and this may serve as a benchmark against which modern multidisciplinary management might be compared.
Article Information
Identifiers and Pagination:
Year: 2008Volume: 2
First Page: 44
Last Page: 50
Publisher Id: TOCCJ-2-44
DOI: 10.2174/1874189400802010044
Article History:
Received Date: 20/2/2008Revision Received Date: 8/4/2008
Acceptance Date: 4/7/2008
Electronic publication date: 1/04/2008
Collection year: 2008
open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http: //creativecommons.org/licenses/by-nc/3.0/ which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
* Address correspondence to this author at the Department of Surgery, William Harvey Hospital, Ashford, TN24 0LZ, Kent; Tel: 01233 750304; Fax: 01233 750599; E-mail: bates.tom@virgin.net
| Open Peer Review Details | |||
|---|---|---|---|
| Manuscript submitted on 20-2-2008 |
Original Manuscript | The Changing Management of Esophageal Carcinoma: Survival in a Population Cohort 1985-1994 | |
INTRODUCTION
In contrast to the incidence of gastric cancer, which has fallen worldwide, the incidence of esophageal cancer has been increasing at an appreciable rate. There has been an increase in the incidence of adenocarcinoma of the distal esophagus, together with a shift of gastric carcinoma from the distal part of the stomach to the cardia and esophago-gastric junction [1-4]. Surgical resection is still the treatment for esophageal carcinoma which gives the best chance of achieving a cure, but this can only be achieved by accurate staging of the disease and may be improved by neo-adjuvant or adjuvant chemo-radiotherapy [2, 3]. The majority of patients diagnosed with upper gastrointestinal cancer only survive a few months after diagnosis because of the insidious nature of the condition but this poor prognosis is not fully reflected in published series of cases referred for surgery. The relatively low incidence of the disease in the UK may also delay presentation and result in the disease being too advanced at presentation for surgical intervention. There was an apparent change in the management of esophageal carcinoma with a more selective approach to surgical resection and an increase in palliation by intubation and radiotherapy in the era before the introduction of modern multidisciplinary management
[5] with intensive staging investigations and the increasing use of chemotherapy. However the evidence for such a trend has been anecdotal and any change in practice and outcome has not been well documented. A ten year cohort study spanning the period of the perceived change of management, 1985-1994, was therefore carried out. The inclusion of all cases of esophageal cancer in a defined population documents the overall survival from the disease in the era preceding current multidisciplinary management.
MATERIALS AND METHODS
Over a ten year period between 1985-1994, all cases of esophageal carcinoma were studied in a Health District with a stable population of approximately 280,000. All death certificates over the period were examined and a computer search of the histopathological data-base was carried out for all cancers of the esophagus and stomach. A hand search was made of the operating theatre logbooks and a hand/computer search of the endoscopy records was also performed. Where possible the hospital records were retrieved and those cases of documented carcinoma of the cardia were included. Details of the histological type and node status were recorded. Cases with carcinoma of the body and distal stomach were excluded.
Details of the type of stent inserted and whether the latter was used in conjunction with chemo- or radiotherapy were recorded. The type of surgical resection and the operating surgeon were recorded. Data on the trends in the catchment population over the period of the study were obtained from the Office for National Statistics [6]. The treatment year and the length of survival were taken from the date of diagnosis. Operative mortality at 30 days was taken from the date of operation. All patients were followed up and at the most recent review of the survivors in October 2005, the minimum length of follow-up was 11 years. Overall and recurrence-free survival following primary treatment with surgery, radiotherapy alone, dilatation/intubation alone or supportive care were compared by Life Table analysis (Kaplan-Meier) and statistical analysis by the log rank test (Medcalc Schoonjans 2005).
RESULTS
A total of 413 patients diagnosed with esophageal carcinoma was identified between 1985 and 1994 of whom 109 had a surgical resection. From 1992 onwards there was a sharp decline in the proportion of patients treated by surgery, (Fig. 1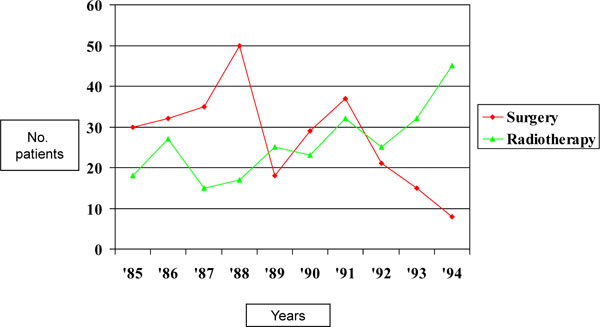 ) although the number of cases increased (Table 1). In the last 2 years of the study only 9 of 84 (11%) patients with esophageal cancer had a surgical resection.
) although the number of cases increased (Table 1). In the last 2 years of the study only 9 of 84 (11%) patients with esophageal cancer had a surgical resection.
There was a corresponding rise in the proportion of patients treated conservatively from 63% up to the end of 1988, to 79% in the subsequent years. The proportion of patients who received radiotherapy with palliative intent (n=92), or in addition to surgery (n=14) also rose over the 10 year period (Fig. 1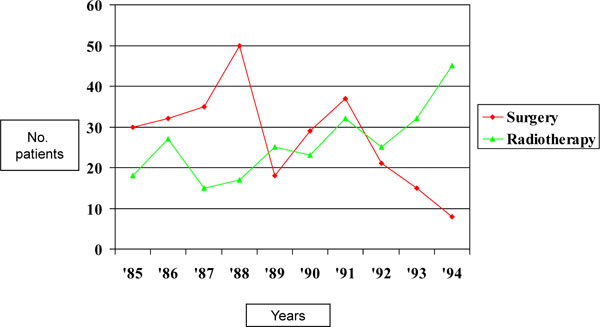 ).
).
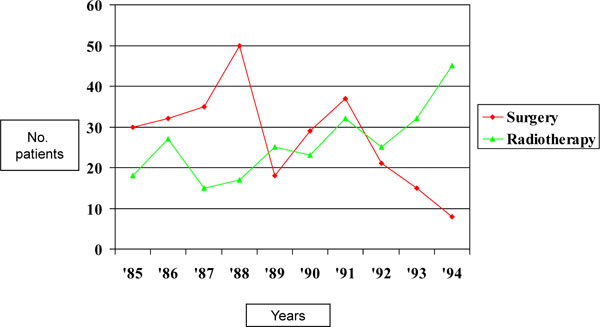 |
Fig. (1) Treatment of patients with esophageal cancer by surgery and radiotherapy over the decade 1985-1994. |
ESOPHAGEAL DILATATION/INTUBATION
Dilatation of esophageal cancers with or without intubation was carried out in 234 patients (Table 1) and in 103 cases this was the sole primary treatment. Palliation with a stent was attempted in 93 patients of which 73% were of Celestin type, 22% Nottingham/Atkinson and 5% were not recorded. No patient in this cohort received intubation with an expandable metal stent.
CHEMOTHERAPY
Chemotherapy was only given to 13 patients which was adjuvant to other treatment in 9 patients but in 4 was the sole primary treatment.
SUPPORTIVE CARE
No active primary treatment was given to 105 patients (25%) who received supportive care. This group included 12 patients where the diagnosis was only confirmed at post mortem and 37 patients where the diagnosis was confirmed but no definitive treatment was given.
SURGICAL RESECTION
Of the 109 patients treated by surgical resection, under the care of four surgeons, 59% underwent transhiatal esophagectomy, 16% an Ivor-Lewis operation, 12% a left thoracic approach, 7% a transabdominal operation for carcinoma of the cardia and in 4% a 3 stage procedure was carried out. In 3 cases the operation record was not available. Adjuvant radiotherapy was given in 14 surgical cases and chemotherapy in 5.
PATHOLOGY
Histological confirmation was confirmed in 93% of cases. In the first two years 1985-1986 the incidence of adenocarcinoma (47%) was similar to squamous cell carcinoma but thereafter adenocarcinoma became predominant (70%).
PREOPERATIVE STAGING
CT scans were not available until the last three years of the study but pre-operative staging by laparoscopy was used to an increasing extent in the later years.
POPULATION ESTIMATE
The office for National Statistics estimated the rise in the catchment population for S.E. Kent over the study period in the age range 70-74 to have been 7% in males and 4.8 % in females [6]. It is unlikely that many patients were referred outside the district for the treatment of esophageal cancer over the period of the study. Only one patient is known to have been referred for resectional surgery in London.
SURVIVAL
Node Status
Of 109 patients who had a surgical resection the nodes were positive in 69 (63%), negative in 36 and not recorded in four. The median survival in the node negative patients was 24 months compared with 11 months for the node positive patients (p<0.001) (Fig. 2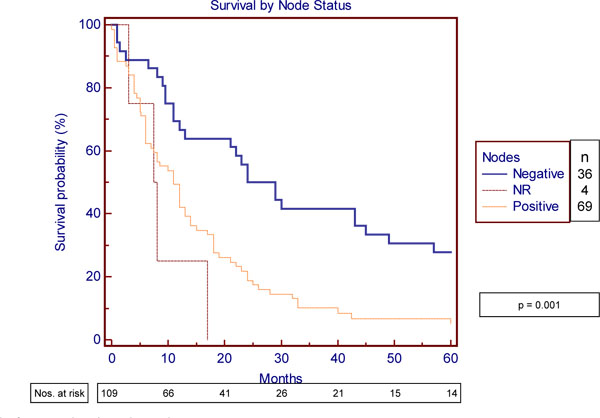 ).
).
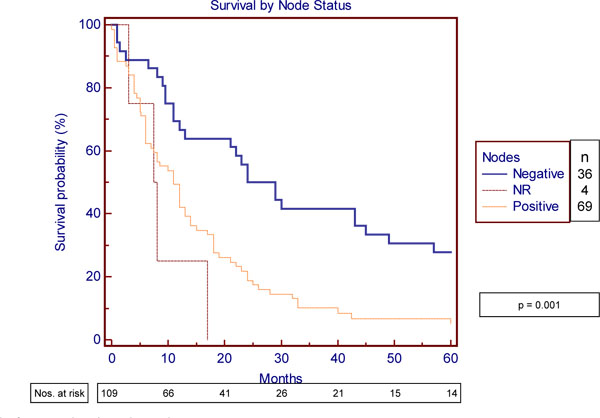 |
Fig. (2) Survival of operated patients by node status. |
The median survival of 109 surgical patients was 12 months, compared with 6 months for the 92 patients treated by palliative radiotherapy. The median survival for the group treated primarily with dilatation/intubation was 3.5 months and for those who received supportive care 1.5 months (Fig. 3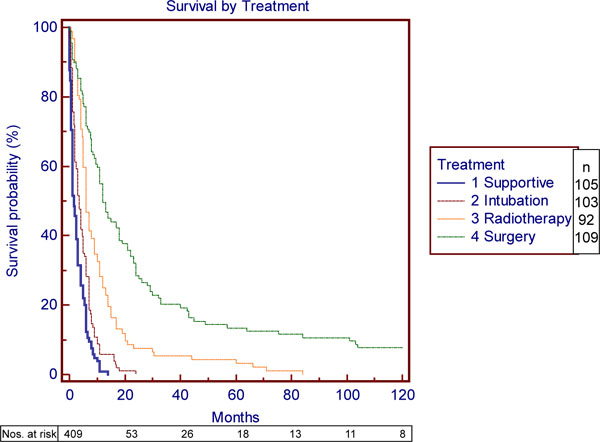 ).
).
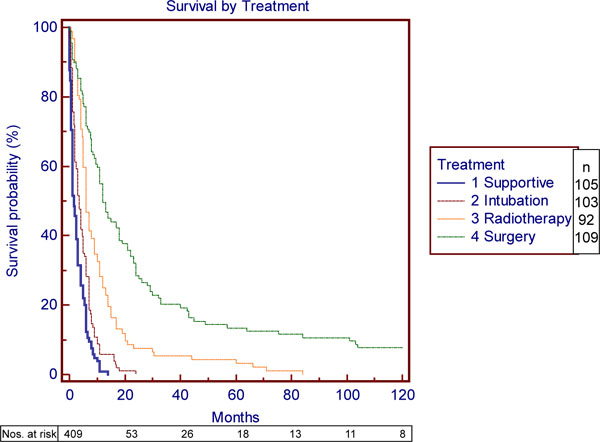 |
Fig. (3) Survival by primary treatment. (This figure does not include 4 patients treated by chemotherapy alone). |
The median survival of the operated patients who had adjuvant radiotherapy (n=14) was 29 months compared with 12 months for those who did not (n=95) but the difference was not significant. (p= 0.22) The median survival of the 13 patients who had chemotherapy was 13 months. Only 15 squamous carcinomas were resected with a median survival of 12 months.
There were more long-term survivors in the later period 1989-94 (7/58) vs 1/51 in the earlier 4 years (p<0.05. Fisher’s exact test), when the proportion of surgical treatment for esophageal cancer was in decline. There was no difference in the overall median survival with the apparent change in the management 1985/88 v. 1989/94. Hazard ratio 0.95 (95% CI = 0.76 to 1.155) (Fig. 4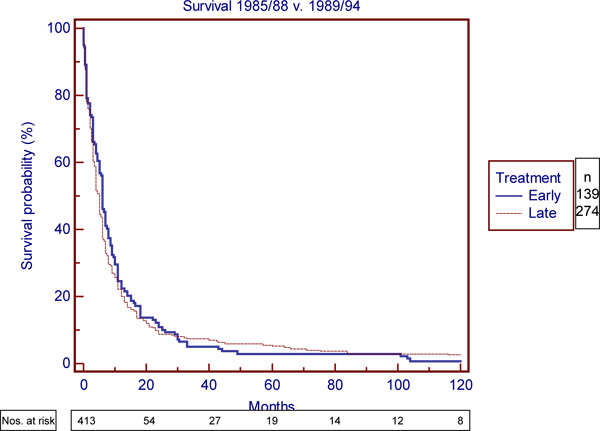 ).
).
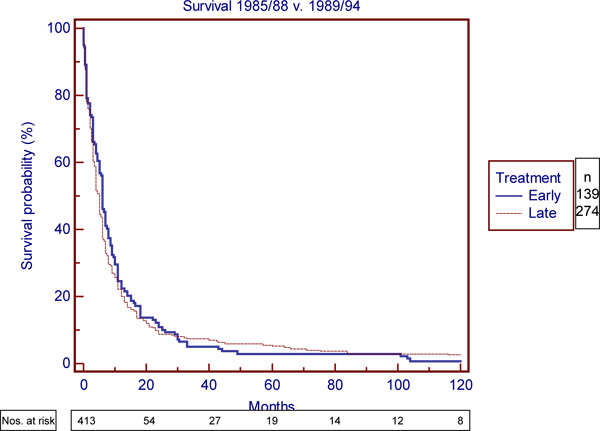 |
Fig. (4) Survival of total cohort 1985/88 vs. 1989/94. |
However, there was a marginal improvement in survival seen in the surgical patients operated on in the later period. The five-year survival rate doubled from 8% to 17.2% and the median survival of 15 months compared with 11 months in the early group 1985/88 p= 0.0502 Hazard ratio 1.46 (95%CI 0.9997 to 2.26) (Fig. 5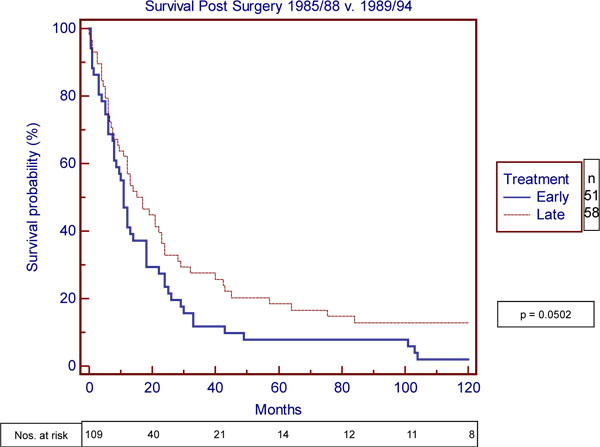 ).
).
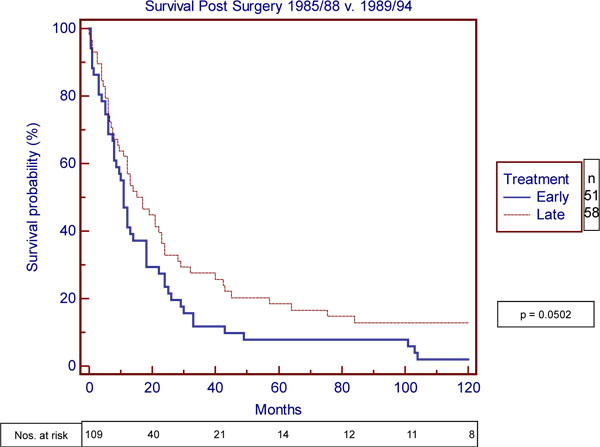 |
Fig. (5) Survival post surgery 1985/88 vs. 1989/94. |
There were 10 post-operative deaths within 30 days (9.3%) but the operative mortality in the early period 1985/88 fell from 6/51 (12%) to 4/58 (6.9%) in the later period. (N.S.) The five year survival rate of the operated patients including post-operative mortality was 12% (13/109).
There were only 8 long-term survivors at 10 years post surgery (7.3%), none of whom had received adjuvant chemotherapy or radiotherapy. One patient was lost to follow-up at 33 months post surgical resection, when clinically free of recurrence. Of the long-term survivors three had a squamous carcinoma and five an adenocar-cinoma. Five patients treated by surgery between 1989 and 1994 were still alive in October 2005 but all non-surgical patients had died.
DISCUSSION
The very few long-term survivors in this total population cohort of patients from the decade 1985-1994 had all been treated by surgery alone. The increasing place of chemotherapy in the treatment of esophageal cancer had not yet been established but his study does document a change in practice towards a more selective management of esophageal cancer with a decline in the rate of surgical resection. The outlook for those patients offered surgery improved and it is likely that the reduction of operative mortality from 12% to 6.9% is largely due to improved intensive care facilities. However, the separation of the survival curves at about 1 year in Fig. (5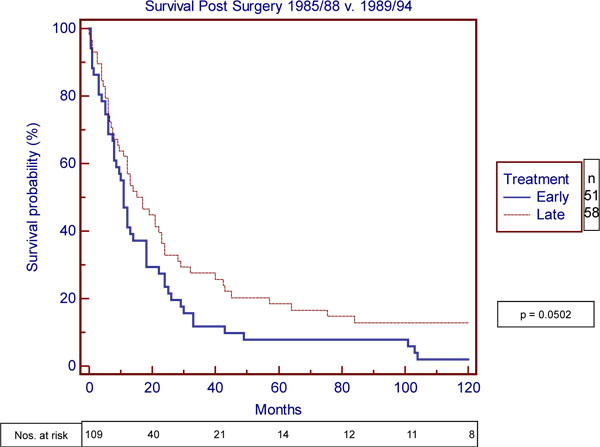 ), in the absence of adjuvant therapy in the long-term survivors suggests that case selection may have improved. CT scans were only available from 1992 and pre-operative staging by laparoscopy was used to an increasing extent in the latter part of the study. It is likely that these two factors largely account for the reduced number of patients offered surgery towards the end of the period (Fig. 1
), in the absence of adjuvant therapy in the long-term survivors suggests that case selection may have improved. CT scans were only available from 1992 and pre-operative staging by laparoscopy was used to an increasing extent in the latter part of the study. It is likely that these two factors largely account for the reduced number of patients offered surgery towards the end of the period (Fig. 1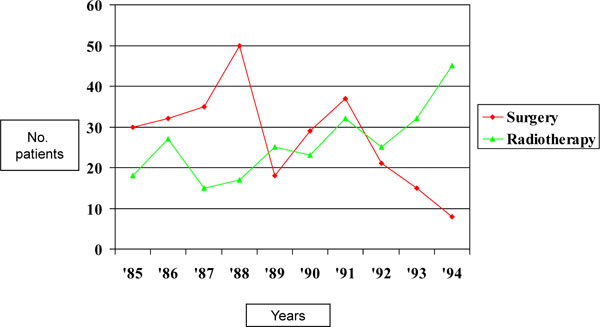 ). Every effort was made to identify all cases of esophageal cancer in the defined population cohort and although it is possible that more patients were referred to specialist centers this was not common practice over this period and any such case is likely to have been identified by the pre-operative biopsy or the death certificate. The few cases diagnosed at post mortem, where this was the certified cause of death, are unlikely to have died from another cause.
). Every effort was made to identify all cases of esophageal cancer in the defined population cohort and although it is possible that more patients were referred to specialist centers this was not common practice over this period and any such case is likely to have been identified by the pre-operative biopsy or the death certificate. The few cases diagnosed at post mortem, where this was the certified cause of death, are unlikely to have died from another cause.
Esophageal Carcinoma in 1985 was the Ninth Most Common Malignancy
Worldwide [5] and the incidence in England and Wales continues to rise. A number of factors have been attributed to this increase in incidence, which include alcohol, smoking, obesity, an increase in Barrett’s oesophagus secondary to reflux disease and the introduction of H2 blockers [1,2,7,8]. A number of potentially curative and palliative treatments exist and although surgical resection has remained the main chance of cure for this condition, treatment has latterly been reinforced by adjuvant chemoradiotherapy [9-12] and most recently with evidence of survival benefit from perioperative chemotherapy [13]. There is now evidence that a high surgical workload improves operative mortality but this is as much a factor of the hospital volume as of the surgeon [14-16] and in the UK this has lead to regionalization of high risk gastrointes-tinal surgery.
A transthoracic three-field lymphadenectomy carries considerable morbidity and since node positive disease has such a poor prognosis, considerable efforts are now made to exclude local extension and node involvement with endoluminal ultrasound [17, 18] and more distant disease with a CT-PET scan [19]. The transhiatal operation has much the same long-term outcome and since this approach carries less morbidity than the transthoracic operation this may have some advantage [20].
Palliative procedures carry their own morbidity and mortality so that quality of life assessment is most important. Blazeby et al. have shown that patients treated with palliation alone have consistently poorer function and more troublesome symptoms [21] but quality of life scores may not predict short-term outcome [22]. Esophagectomy does not always give good palliation especially when the mean survival was only 12 months but quality of life data were not available for the current cohort of patients.
The present study confirms that there was a definite change in management of esophageal cancer with fewer surgical resections and an increase in palliative treatment over the ten year period 1985-94. Palliation mainly took the form of intubation with the previous generation of rigid plastic tubes [23] or radiotherapy and very few patients received chemotherapy. There was no change in consultant medical or surgical staff over the study period but although they did not function as a multidisciplinary team at this time, a gradual change in practice has been confirmed.
Over the ten year period of study both the male and female population increased by 7.3% and 4.8% respectively for 70-74 year age group which would indicate that there were more people at risk of developing esophageal carcinoma in the latter part of the study. One would therefore have expected to see an increase in the number of patients having surgery but this was not the case.
The reported operative mortality and 5 year survival of esophagectomy vary widely but the nearest series to the present study is a Finnish cancer registry based population cohort of 402 patients with adenocarcinoma diagnosed between 1990 and 1998 [24]. The operation rate of 42.5% was higher than the rate of 27% in the present series and although the operative mortality was similar at 8.8% the 5 year survival was higher at 29% v. 12%. The operative mortality of transhiatal esophagectomy within the present study was 5.9% [25].
Thirty day operative mortality as low as 1.1 % has been reported from France [26] with a 5 year survival of 59%. However, this was a series with 78% squamous carcinoma and only 29% node positive cases. The present study more closely matches the data from Southampton [27] and Australia [28]. In the former study, for 1974-1996 the in-hospital mortality fell from 8.8% to less than 5% but the 5 year survival remained disappointingly low at 15.3% compared with 17% in the latter part of the present study.
The trend towards more careful selection of patients for surgery has not been the result of randomised controlled trials or prospective studies but reflects a change of practice in the light of a poor outcome for many patients [29, 30]. The short median survival of 11 months for node positive patients who had a surgical resection underlines the need to identify this group as far as possible by imaging techniques before surgery is considered. It is clear that the multidisciplinary team approach has further improved the staging accuracy and care of esophageal cancer [31, 32] and there is some evidence from historical controls that it has improved outcome [33, 34]. Modern therapy has substantially improved the outcome for operable esophageal cancer but the present study may serve as a benchmark when all cases presenting in a defined population are considered