- Home
- About Journals
-
Information for Authors/ReviewersEditorial Policies
Publication Fee
Publication Cycle - Process Flowchart
Online Manuscript Submission and Tracking System
Publishing Ethics and Rectitude
Authorship
Author Benefits
Reviewer Guidelines
Guest Editor Guidelines
Peer Review Workflow
Quick Track Option
Copyediting Services
Bentham Open Membership
Bentham Open Advisory Board
Archiving Policies
Fabricating and Stating False Information
Post Publication Discussions and Corrections
Editorial Management
Advertise With Us
Funding Agencies
Rate List
Kudos
General FAQs
Special Fee Waivers and Discounts
- Contact
- Help
- About Us
- Search

The Open Medical Informatics Journal
(Discontinued)
ISSN: 1874-4311 ― Volume 13, 2019
Tele-ICU: Efficacy and Cost-Effectiveness Approach of Remotely Managing the Critical Care
Sajeesh Kumar*, Shezana Merchant , Rebecca Reynolds
Abstract
Tele-ICU has an off-site command center in which a critical care team (intensivists and critical care nurses) is connected with patients in distance intensive care units (ICUs) through a real-time audio, visual and electronic means and health information is exchanged. The aim of this paper is to review literature to explore the available studies related to efficacy and cost effectiveness of Tele-ICU applications and to study the possible barriers to broader adoption. While studies draw conclusions on cost based on the mortality and Length of Stay (LOS), actual cost was not reported. Another problem in the studies was the lack of consistent measurement, reporting and adjustment for patient severity. From the data available, Tele-ICU seems to be a promising path, especially in the United States where there is a limited number of board-certified intensivists.
Article Information
Identifiers and Pagination:
Year: 2013Volume: 7
First Page: 24
Last Page: 29
Publisher Id: TOMINFOJ-7-24
DOI: 10.2174/1874431101307010024
Article History:
Received Date: 26/7/2012Revision Received Date: 22/9/2012
Acceptance Date: 23/9/2012
Electronic publication date: 23 /8/2013
Collection year: 2013
open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
* Address correspondence to this author at the Department of Health Informatics & Information Management, University of Tennessee Health Science Center,920 Madison Avenue Suite 518, Memphis, Tennessee 38163, USA; Tel: 901-448-2125; Fax: 901-448-1629; E-mail: skumar10@uthsc.edu
| Open Peer Review Details | |||
|---|---|---|---|
| Manuscript submitted on 26-7-2012 |
Original Manuscript | Tele-ICU: Efficacy and Cost-Effectiveness Approach of Remotely Managing the Critical Care | |
INTRODUCTION
There is a shortage of Intensivists in the United States, and the demand for them is only going to get worse with the aging population [1Mullen-Fortino M, DiMartino J, Entrikin L, Muliner S, Hanson CW, Kahn JM. Bedside nurses' perceptions of intensive care unit telemedicine Am J Crit Care 2012; 21: 24-32.]. As of 2010, less than 15% of Intensive Care Units (ICU) are able to provide intensivist care [2Goran S. A second set of eyes: an introduction to tele-ICU Crit Care Nurse 2010; 30(4): 46-54.]. There are 6000 ICUs but only 5500 board-certified intensivists [3Ries M. Tele-ICU A new paradigm in critical care Int Anesthesiol Clin 2009; 47(1): 153-70.]. Studies have shown that hospitals with a dedicated intensivist on staff had a significant reduction in ICU mortality and average Length of Stay (LOS) [4Celi LA, Hassan E, Marquardt C, Breslow M, Rosenfeld B. The eICU: It's not just telemedicine Crit Care Med 2001; 29(8): N183-9., 5Morrison JL, Cai Q, Davis N, et al. Clinical and economic outcomes of the electronic intensive care unit: Results from two community hospitals Crit Care Med 2010; 38(1): 2-8.]. Complexity of today’s ICU services emphasizes the need for sharing health information through off-site ICU centers [6Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985-2000: An analysis of bed numbers, use, and costs Crit Care Med 2004; 32(6): 1254-9.]. Tele-ICU is the use of health information exchanged from hospital critical care unit to another via electronic communications [7Grundy BL, Jones PK, Lovitt A. Telemedicine in critical care: problems in design. implementaion.and assessment Crit Care Med 1982; 10(7): 471-5.]. Tele-ICU intensivists provide real-time services to multiple care centers regardless of their locations. Tele-ICU has an off-site command center in which a critical care team (intensivists and critical care nurses) is connected with patients in distant ICUs through a real-time audio, visual and electronic means. Similar to a bedside team, offsite Tele-ICU intensivists require full access to patient data. Tele -ICU is capable of providing: a real time monitoring of patient instability or any abnormality in laboratory, order diagnostics tests, making diagnosis and order treatment, implementing any intervention through controlling life support devices. As a result, Tele-ICU holds great promise in improving the quality of critical care patients and increasing the productivity of intensivists. This paper aims to explore the available studies related to efficacy and cost effectiveness of Tele-ICU applications and to outline possible barriers to broader adoption.
METHODS
Electronic databases were searched to identify relevant articles. Searches were limited to the English language and the earliest available publication date for each database to March 2012. PubMed/Medline, EMBASE, CINAHL with Full Text, PsychINFO, EBM Reviews (e.g. Cochrane Database of Systematic Reviews, ACP Journal Club, Database of Abstracts of Reviews of Effects, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register, Health Technology Assessment, and NHS Economic Evaluation Database), Scopus, Education Resource Information Center (ERIC), and Turning Research into Practice (TRIP) were used to conduct the literature searches. Searches used subject headings and subheadings if available and were combined with keywords. Search terms used included telehealth, benefits of tele-ICU, tele-ICU outcomes, telemedicine in the ICU and tele-ICU cost.
Selection Criteria
The article was included if 1) it pertained to uses of telemedicine in ICU; 2) Assessed the outcome of implementing Tele-ICU through measuring its effect on mortality rate and on length of stay (LOS); 3) Explored the staff attitude toward implemented Tele-ICU. Articles not relevant to the topic were excluded. Potential eligibility of the articles was first determined from the title and abstracts identified from the searches. Full-text articles were then retrieved and evaluated for relevance. Articles were excluded at this point if they were not found to meet the above criteria once the full text was examined (for flow chart of article retrieval see Fig. 1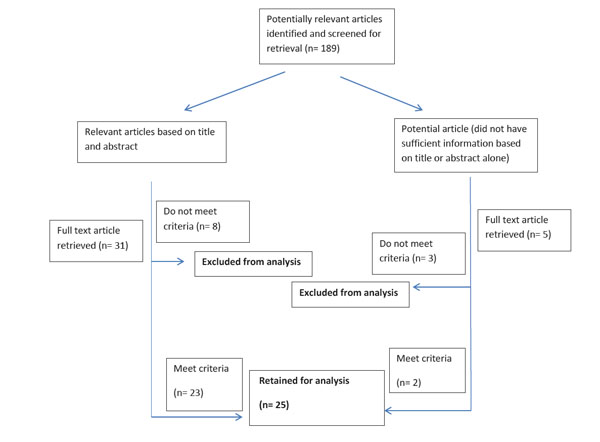 ). A second researcher confirmed the relevance and findings from the selected articles.
). A second researcher confirmed the relevance and findings from the selected articles.
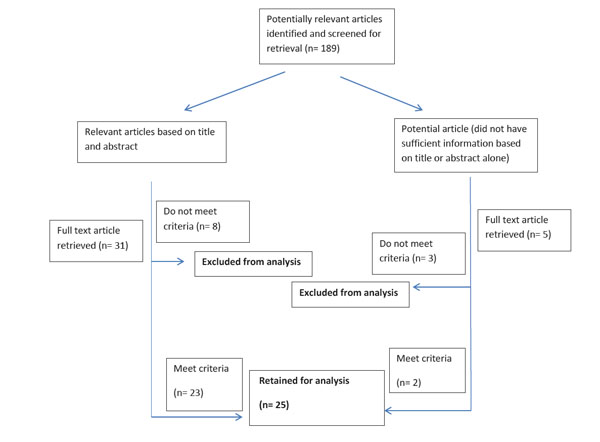 |
Fig. (1) Flow chart of the results from the literature search. |
Data Extraction and Outcome Measures
The articles were reviewed and a data extraction form was used to include details pertaining to the study quality such as study design, number of subjects, study population, as well as the description of the program. The acute nature of ICU and the high cost associated with critically ill patients makes the survival rate and the cost saving among the most desirable outcomes measured. Consequently, integration of distance monitoring and observation of intensivists’ services to bedside care were significant outcome measures along with the mortality rate and length of stay. The following types of outcomes reported that were of interest for this review were recorded: (1) Clinical process: Outcomes related to service delivery, such as attendance and adherence to programs and recommendations, as well as healthcare provider and staff satisfaction with the program; (2) Healthcare utilization: Events that occur outside the program’s scope and that the program may aim to reduce or increase, such as hospitalizations, ICU admissions and average Length of Stay;(3) Costs: From the patient’s, provider’s or organization’s perspective, all costs (savings and/or expenses) associated with the use of Tele-ICU.
RESULTS
As Fig. (1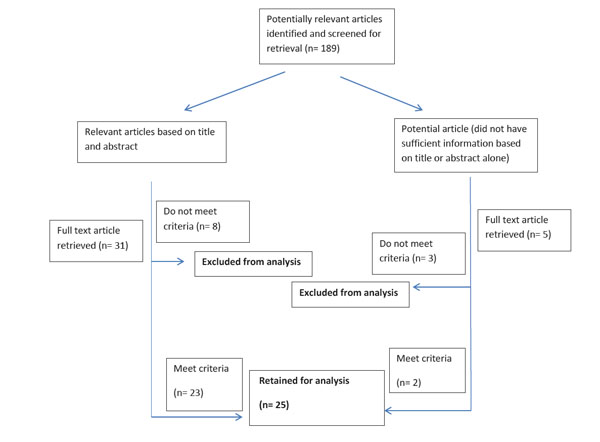 ) indicates, 25 studies were retained after the initial screening of titles and abstracts and the full-text retrieval of pertinent articles. The results of the clinical process outcomes, healthcare utilization and costs reported in the studies are presented in the following sections.
) indicates, 25 studies were retained after the initial screening of titles and abstracts and the full-text retrieval of pertinent articles. The results of the clinical process outcomes, healthcare utilization and costs reported in the studies are presented in the following sections.
Clinical Adoption of Tele-ICU
Tele-ICU as a concept is evolving over time; the approach used in the 1970s and later involved a video connection between the bedside care providers and outside consultants without any access to patient monitoring data. The most frequent adopted approach today is the continuous access and monitoring care that focuses on providing supplemental critical care expertise [8Goran SF, Van der Kloot T. Savings in RN staffing costs pre and post eICU implementation In: eICU Program Success Stories Baltimore MD: Philips-VISICU 2008.-13Waheed A. NEHI, 2010 and AHA Annual Survey of Hospitals for FY07, and AHA Annual Survey of Hospitals for FY06 2010; 00: 0.]. In 2000, Sentara hospital was the first hospital to implement the new Tele-ICU approach. As of 2011, 41 ICU command centers have been installed with a total of 5789 ICU beds being covered throughout 249 hospitals [13Waheed A. NEHI, 2010 and AHA Annual Survey of Hospitals for FY07, and AHA Annual Survey of Hospitals for FY06 2010; 00: 0.]. Even with the early positive impacts of Tel-ICU, there are only 5-7% of adult ICU beds covered by this technology in the USA [13Waheed A. NEHI, 2010 and AHA Annual Survey of Hospitals for FY07, and AHA Annual Survey of Hospitals for FY06 2010; 00: 0.]. Adoption of Tele-ICU is greatly obstructed by the lack of documented outcomes and unproven return on investment (ROI) [13Waheed A. NEHI, 2010 and AHA Annual Survey of Hospitals for FY07, and AHA Annual Survey of Hospitals for FY06 2010; 00: 0.]. Moreover, some Tele-ICU centers have deactivated for reasons like physicians resistance to change in both patient’s management and required sharing control over patient with other off-site physicians. Technical difficulties with lack of training could also be other impediments [13Waheed A. NEHI, 2010 and AHA Annual Survey of Hospitals for FY07, and AHA Annual Survey of Hospitals for FY06 2010; 00: 0.].
Barriers to Tele-ICU
Tele-ICU is relatively new; many bedside doctors and nurses do not understand how the system works. They believe that the eRNs and e-intensivists are watching over them and trying to taking over [1Mullen-Fortino M, DiMartino J, Entrikin L, Muliner S, Hanson CW, Kahn JM. Bedside nurses' perceptions of intensive care unit telemedicine Am J Crit Care 2012; 21: 24-32.]. In reality, “the purpose of the system is to provide improved safety through redundancy and enhance outcomes through standardization” [2Goran S. A second set of eyes: an introduction to tele-ICU Crit Care Nurse 2010; 30(4): 46-54.]. The tele-ICU team has a supportive role; they have an overview of what is going on with all the patients in the unit and can alert the bedside staff if any problems occur [14Stafford TB, Myers MA, Young A, Foster JG, Huber JT. Working in an eICU unit: Life in the box Crit Care Nurs Clin North Am 2008; 20: 441-50.]. “The hospital admitting physician continued to be the attending and was responsible for establishing the care plan,” while the TeleICU staff were the primary contact for the on-site nurses [15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8.]. Studies show that the more proactive the Tele-ICU physicians are, “the more improved are the outcomes” [16Willmitch B, Golembeski S, Kim SS, Nelson LD, Gidel L. Clinical outcomes after telemedicine intensive care unit implementation Crit Care Med 2012; 40(2): 450-545.].
Another barrier to ICU telemedicine is the clinician’s acceptance of the technology. This could be one of the reasons that some studies did not show improvement in LOS and mortality in ICU patients. In a study done by Thomas, et al. [17Thomas EJ, Lucke JF, Wueste L, Weavind L, Patel B. Association of telemedicine for remote monitoring of intensive care patients with mortality. complications and length of stay. JAMA 2009; 302(24): 2671-8.], “two-thirds of the patients in our study had physicians who chose minimal delegation to the Tele-ICU.” Other clinicians feel that everything is running perfectly and nothing needs to be fixed. Showing these physicians comparative data and the benefits of Tele-ICU may change their mind [4Celi LA, Hassan E, Marquardt C, Breslow M, Rosenfeld B. The eICU: It's not just telemedicine Crit Care Med 2001; 29(8): N183-9.].
The lack of integration was a problem at some hospitals, especially those that did not have electronic records. Thomas, et al. [7Grundy BL, Jones PK, Lovitt A. Telemedicine in critical care: problems in design. implementaion.and assessment Crit Care Med 1982; 10(7): 471-5.] observed that although the Tele-ICU team had real time access to most of the patient’s information, the monitored unit did not share clinical notes or computerized physician order entry; instead, these notes were faxed daily. Similarly, Berenson et al. [18Berenson RA, Grossman JM, November EA. Does telemonitoring of patients--the eICU--improve intensive care? Health Affairs 2009; 28(5): 937-47.] also noted the limitations related to the lack of interoperability.
Outcome Assessments
With optimizing the telemedicine application in ICU, both the mortality rate and length of stay could influence positively; a 15-60% reduction in the mortality rate along with a 30% reduction in the average length of stay was observed in a hospital with intermittent remote consultation in the delivery of health services to critical care patients. A review of available published articles is presented in Table 1.
The results from the articles were mixed regarding the mortality rate and LOS in ICU after the adoption of ICU telemedicine. For example, according to Thomas, et al. [17Thomas EJ, Lucke JF, Wueste L, Weavind L, Patel B. Association of telemedicine for remote monitoring of intensive care patients with mortality. complications and length of stay. JAMA 2009; 302(24): 2671-8.] “remote monitoring of ICU patients was not associated with an overall improvement in mortality or LOS.” On the other hand, Lilly, et al. [19Lilly CM, Cody S, Zhao H, et al. Hospital mortality. length of stay and preventable complications among crtically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 2011; 305(21): 2175-83.], found that “Tele-ICU intervention was associated with reduced adjusted odds of mortality and reduced hospital length of stay.” Young, et al. [20Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM. Impact of telemedicine intensive care unit coverage on patient outcomes Arch Int Med 2011; 171(6): 498-506.] concluded that Tele-ICU was associated with a decrease in mortality and LOS in the ICU but not within the hospital. A study done by Morrison, et al. [5Morrison JL, Cai Q, Davis N, et al. Clinical and economic outcomes of the electronic intensive care unit: Results from two community hospitals Crit Care Med 2010; 38(1): 2-8.] concluded that a difference in mortality could not be determined because the mortality rate at the hospital was already low in the ICU. Lilly, et al. [19Lilly CM, Cody S, Zhao H, et al. Hospital mortality. length of stay and preventable complications among crtically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 2011; 305(21): 2175-83.] found that after the intervention of Tele-ICU, tools were developed for real-time auditing and reconciliation which increased the adherence to best practices. This also led to a decrease in the rates of complications in the ICU.
Telemedicine in the ICU may also prevent intensivist and nurse “burn outs and posttraumatic stress” [3Ries M. Tele-ICU A new paradigm in critical care Int Anesthesiol Clin 2009; 47(1): 153-70.]. Physicians who are tired due to long hours or stress are more prone to making mistakes. “The Tele-ICU is the “second set of eyes” that provide additional clinical surveillance and support” [10Thomas EJ, Lucke JF. Association of telemedicine for remote monitoring of intensive care patients with mortality. complicatons.and length of stay JAMA 2009; 302(24): 2671-8.]. It has also helped residents that were new to the field [3Ries M. Tele-ICU A new paradigm in critical care Int Anesthesiol Clin 2009; 47(1): 153-70.].
Costs
Adoption of Tele-ICU requires a substantial up-front capital investment with ongoing cost of operation and maintenance. These costs may impede the adoption of this technology especially with lack of reimbursement and uncertainties about return on investment (ROI) calculations. Moreover, the ROI was merely calculated using the indirect clinical effects and the expected length of stay reduction.
Pay-back period or Net Present Value (NPV) are the indictors used for return on investment. More specifically, the equation of financial issue related to tele-ICU is desired to be as the following [15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8.].
[Capital Cost+ Operating Cost] ≤ [Revenue from reimbursement + Cost Saving Attained]
The cost of Tele-ICU varies depending on the setting, hardware, software, training and compatibility issues with other systems. One study reported a cost of over $2 M to set a command center and its components [15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8.]. In general, an estimation of $ 2-5 million is probably the cost to set up a command center and install the Tele- ICU systems with an operation cost of $600,000-1.5 M per year as an operation cost is reported from different adaptors [15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8.].
On the revenue side, one study indicated that there was a 10% reduction in ICU length of stay with ability to care for one new ICU patient per day which could result in a positive $2.5 M net present value (NPV) [15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8.].
Most studies reviewed, used the LOS and mortality to determine cost savings. For example, according to Rosenfeld, et al. [21Rosenfeld BA, Dorman T, Breslow MJ, et al. Intensive care unit telemedicine: Alternate paradigm for providing continuous intensivist care Crit Care Med 2000; 28(12): 3925-1.]. ICU costs decreased between 25% and 31% during the intervention period and hospital costs decreased by 12% to 19%. Breslow, et al. [15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8.]. hired an independent consulting firm to determine the financial outcome of the Tele-ICU program. They determined the cost of care per day of service and also included equipment cost, staff cost and other costs associated with having a Tele-ICU system. The report showed that there was a 24.6% decrease in variable costs per case. This decrease is probably due to a shorter LOS in the ICU and improved clinical outcomes [4Celi LA, Hassan E, Marquardt C, Breslow M, Rosenfeld B. The eICU: It's not just telemedicine Crit Care Med 2001; 29(8): N183-9., 15Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intesivist staffing Crit Care Med 2004; 32(1): 31-8., 21Rosenfeld BA, Dorman T, Breslow MJ, et al. Intensive care unit telemedicine: Alternate paradigm for providing continuous intensivist care Crit Care Med 2000; 28(12): 3925-1.].
Staff Acceptance of Tele-ICU
Implementation of Tele-ICU encompasses a change in the practice of many health workers. Most studies that measured the acceptance of Tele-ICU showed high acceptance for the increased ICU coverage. Moreover, Tele-ICU has a favorable impact on both patient care and on organizations. Thomas et al. [22Thomas EJ, Chu-Weininger MYL, Lucke J. The impact of a tele-ICU on provider attitudes about teamwork and safety climate Crit Care Med 2007; 35: 529.] conducted a pre/post attitude survey for physicians and found that the safety attitudes significantly increased after implementation. Tele-ICU, also increased the confidence that patients were adequately covered. Another study conducted by Kowitlawakul et al. [23Kowitlawakul Y. Technology Acceptance Model predicting nurses acceptance of telemedicine technology (eICU) 2008.]. measured the nurse’s attitude through a survey; it revealed that Tele-ICU would be beneficial in units without adequate physician coverage. Weininger et al. [24Chu-Weininger M. The impact of a tele-ICU on provider attitudes about teamwork and safety climate Qual Saf Health Care 2010; 19(6): e39.] measured the teamwork and safety environment of three ICUs before and after implementation. Their results showed that implementation of a Tele-ICU improved teamwork and the safety climate in some units especially among nurses. As a result, collaboration needed to enhance the value of the Tele-ICU system is acquired through effective implementation of continuous change management plan. With implementing best practice protocols and other quality assurance measures, the scope of Tele-ICU is expected to evolve and extend to other microsystems such as emergency departments, risk delivery unit, long term acute hospital and other departments that are designated to provide immediate response to patients.
DISCUSSION
From the articles reviewed, current studies are early steps but more research needs to be done before Tele-ICU will become more widespread. Some studies did not show any difference pre- and post- adoption because they already had optimal outcomes (see Table 1). Other studies showed a large decrease in LOS and mortality which could be attributed to the fact that the hospital was an open system (Table 1). Similarly, Yoo and Dudley [25Yoo EJ, Dudley RA. Evaluating telemedicine in the ICU JAMA 2009; 302(24): 2705-6.] also found heterogeneity in Tele-ICU systems and believe that “it is unlikely that any single study can definitely address the benefits of telemedicine for the critically ill.” They also mentioned that there is a “lack of consistent reference in the literature to a unifying conceptual framework of what ICU care is and how Tele-ICU could improve it” [25Yoo EJ, Dudley RA. Evaluating telemedicine in the ICU JAMA 2009; 302(24): 2705-6.].
Another problem in the studies was the lack of consistent measurement, reporting and adjustment for patient severity [20Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM. Impact of telemedicine intensive care unit coverage on patient outcomes Arch Int Med 2011; 171(6): 498-506.]. This could have led to inflated results relating to mortality and LOS. One hospital may be a Trauma 1 center and experience many deaths, while another facility could be a smaller hospital that does not typically see those type of patients. Cost-effectiveness is another area that more research needs to be done. While many studies draw conclusions on cost based on the mortality and LOS, actual cost was not reported. This is an important consideration especially for smaller facilities that want to make sure that they will get a return on their investment.
LIMITATIONS OF THIS REVIEW
One of the limitations of this systematic review is that it uses studies published in a peer-reviewed journal. It is well documented that there is a publication bias towards studies that have positive findings [39Egger M, Smith GD, Sterne JA. Uses and abuses of metaanalysis Clin Med 2001; 1(6): 478-.]. Therefore, studies that do not demonstrate any effect or report a negative effect of Tele-ICU may not carry as much weight in the synthesis of the data because they were not identified through the search. Moreover, this study did not include studies looking at patient assessment as the focus of this review was on Tele -ICU intervention program. This was a first attempt to identify scientifically sound evidence of telemedicine intervention program and synthesize and critically appraise the published literature in this area. In part this also helps identify possible directions for future studies.
CONCLUSION
This systematic review identified a substantial amount of scientific literature in the relatively new area of Tele-ICU. This review showed that although there is heterogeneity between studies in terms of study designs, settings and outcomes measured, there is a consistent trend in the literature supporting the efficacy and effectiveness of Tele-ICU. In conclusion, from the data available, Tele-ICU seems to be a promising path, especially in the United States where there is a limited number of board-certified intensivists.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.



