- Home
- About Journals
-
Information for Authors/ReviewersEditorial Policies
Publication Fee
Publication Cycle - Process Flowchart
Online Manuscript Submission and Tracking System
Publishing Ethics and Rectitude
Authorship
Author Benefits
Reviewer Guidelines
Guest Editor Guidelines
Peer Review Workflow
Quick Track Option
Copyediting Services
Bentham Open Membership
Bentham Open Advisory Board
Archiving Policies
Fabricating and Stating False Information
Post Publication Discussions and Corrections
Editorial Management
Advertise With Us
Funding Agencies
Rate List
Kudos
General FAQs
Special Fee Waivers and Discounts
- Contact
- Help
- About Us
- Search

The Open Virology Journal
(Discontinued)
ISSN: 1874-3579 ― Volume 15, 2021
Evidence and Impact of Human Papillomavirus Latency
Patti E Gravitt*
Abstract
At present, there is no consensus in the scientific community regarding the ability for human papillomavirus (HPV) infections to establish latency. Based on animal studies, a model of papillomavirus latency has been proposed in which papillomaviruses can be retained in the basal epithelial stem cell pool as latent infections and periodically induced to reactivate when the stem cell divides and one daughter cell is committed to terminal differentiation and induction of the viral life cycle. Tissue resident memory T-cells are hypothesized to control these periodic reactivation episodes and thus limit their duration. In this paper, evidence from human studies consistent with this model of papillomavirus latency is reviewed. Given the strong circumstantial evidence supporting a natural history of HPV infection which includes a immunologically controlled latent state, the longer term implications of HPV latency on a highly infected and aging population may warrant a more serious evaluation.
Article Information
Identifiers and Pagination:
Year: 2012Volume: 6
Issue: Suppl 2
First Page: 198
Last Page: 203
Publisher Id: TOVJ-6-198
DOI: 10.2174/1874357901206010198
Article History:
Received Date: 12/6/2012Revision Received Date: 13/9/2012
Acceptance Date: 17/9/2012
Electronic publication date: 28/12/2012
Collection year: 2012
open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http: //creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
* Address correspondence to this author at the Perdana University Graduate School of Medicine, Jalan MAEPS Perdana, Serdang, Selangor MY 43400, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St., Baltimore, MD 21205, USA; Tel: 443-287-6179; Fax: 410-955-1383; E-mail: pgravitt@jhsph.edu
| Open Peer Review Details | |||
|---|---|---|---|
| Manuscript submitted on 12-6-2012 |
Original Manuscript | Evidence and Impact of Human Papillomavirus Latency | |
INTRODUCTION
Viral latency, as defined by Siliciano and Greene, "is a state of reversibly nonproductive infection of individual cells" [1 Siliciano RF, Greene WC. HIV Latency Cold Spring Harb Perspect Med 2011; 1(1 ): a007096.]. Despite the rapid progress made in characterizing the large family of papillomaviruses and their etiology in several human cancers, there is still uncertainty regarding the existence of a latent state in human papillomavirus infections. According to Fields Virology, "It is known that HPV can establish latency" [2Knipe DM, Howley PM, Eds. Howley and Lowy, Chapter 62. Papillomaviruses Fields Virology. 5th. Philadelphia: Lippincott: Williams and Wilkins 2007.]. However, a review of clinical and epidemiological literature uncovers a less certain perspective.
Recently, a new model of human papillomavirus (HPV) latency was proposed based on the evidence derived from models of rabbit oral papillomavirus infection (ROPV) [3 Maglennon GA, McIntosh P, Doorbar J. Persistence of viral DNA in the epithelial basal layer suggests a model for papillomavirus latency following immune regression Virology 2011; 414(2 ): 153-63.]. This model proposes that, under a model of asymmetric epithelial cell replacement, each HPV infected basal stem cell will divide with a 1: 1 replication and division of viral episome. One infected daughter cell will enter the supra basal layers committed to terminal differentiation and induction of HPV viral replication, while the other infected daughter cell will remain quiescent in the basal epithelial stem cell pool. Under this model, the first component of the definition of viral latency - a state of non-productive infection of individual cells - appears to be met, since productive PV infection cannot occur in the absence of terminal differentiation. Thus, it is likely that the HPV-infected daughter cell that remains in the epithelial stem cell pool is the site of HPV latency. The second condition to meet the definition of viral latency is reversibility. The current model of PV latency predicts that this can readily occur anytime a latently infected, quiescent basal stem cell is induced to divide. At this time, it is anticipated that one infected daughter cell will be committed to terminal differentiation and renewed viral replication. However, the other daughter cell would be expected to again be retained in the epithelial stem cell pool, a life cycle which, in the absence of major external factors, would ensure lifelong HPV carriage.
EPIDEMIOLOGICAL EVIDENCE OF HPV REACTIVATION
Despite the expressed skepticism for a latent state in the natural history of HPV infection, recent epidemiological literature is quite consistent with a model of latency. Because there is constant turnover of the cervical epithelium, the model of epithelial stem cell latency would predict periodic recurrence of HPV detection. Epidemiological evidence supports this prediction [4 Trottier J, Ferreira S, Thomann P, et al. Human papillomavirus infection and reinfection in adult women the role of sexual activity and natural immunity Cancer Res 2010; 70(21 ): 8569-77.-7 Rodriguez AC, Schiffman M, Herrero R, et al. Low risk of type-specific carcinogenic HPV re-appearance with subsequent cervical intraepithlelial neoplasia grade 2/3 Int J Cancer 2012; 131(8 ): 1874-81.] (Table 1). In these studies, women observed to have cleared a specific HPV genotype during the study period were evaluated for the probability of recurrent detection of the same genotype. Recurrent detection was observed in all studies, ranging from 3.3% for HR-HPV recurrence in the Ludwig-McGill cohort study (Brazil) [4 Trottier J, Ferreira S, Thomann P, et al. Human papillomavirus infection and reinfection in adult women the role of sexual activity and natural immunity Cancer Res 2010; 70(21 ): 8569-77.] to 19.4% in a study of college-aged women in Washington State (USA) [6 Winer RL, Hughes JP, Feng Q, et al. Early natural history of incident, type-specifi human papillomavirus infections in newly sexually active young women Cancer Epidemiol Biomarkers Prev 2011; 20(4 ): 699-707.]. In all studies, the authors acknowledge that there could be several alternative explanations for these observations besides latent virus reactivation. First, these could represent new infections (or re-infection) with the same genotype. However in 2 of the 3 studies which evaluated this [5 Insinga RP, Perez G, Wheeler CM, et al. Incidence, duration, and reappearance of type-specific cervical human papillomavirus infections in young women Cancer Epidemiol Biomarkers Prev 2010; 19(6 ): 1585-94., 7 Rodriguez AC, Schiffman M, Herrero R, et al. Low risk of type-specific carcinogenic HPV re-appearance with subsequent cervical intraepithlelial neoplasia grade 2/3 Int J Cancer 2012; 131(8 ): 1874-81.], no association was observed between recurrent type-specific detection and report of a new sexual partner, and one study reported that recurrent detections of HPV16 were confirmed to have identical sequence compared with the original HPV16 detection [6 Winer RL, Hughes JP, Feng Q, et al. Early natural history of incident, type-specifi human papillomavirus infections in newly sexually active young women Cancer Epidemiol Biomarkers Prev 2011; 20(4 ): 699-707.]. In addition, several studies have reported rates of 'incident' infection among sexually abstinent women that are similar to the recurrence rates reported in the studies in Table 1, suggesting that at least a fraction of these infections cannot be explained by acquisition from a male partner [7 Rodriguez AC, Schiffman M, Herrero R, et al. Low risk of type-specific carcinogenic HPV re-appearance with subsequent cervical intraepithlelial neoplasia grade 2/3 Int J Cancer 2012; 131(8 ): 1874-81.-9 Theiler RN, Farr SL, Karon JM, et al. High-risk human papillomavirus reactivation in human immunodeficiency virus-infected women: risk factors for cervical viral shedding Obstet Gynecol 2010; 115: 1150-8.]. Alternatively, these results could have occurred by simple misclassification (i.e., false positive or false negative results). The study reported by Insinga et al. [5 Insinga RP, Perez G, Wheeler CM, et al. Incidence, duration, and reappearance of type-specific cervical human papillomavirus infections in young women Cancer Epidemiol Biomarkers Prev 2010; 19(6 ): 1585-94.], was able to evaluate the likelihood of these explanations quite carefully. In this study, endo/ectocervical swabs provided the primary outcome measure, but a second labial/vulvar/perineal/perianal (LVPP) swab was taken concomitantly and was analyzed for type specific concordance with the cervical swab. At least some type-specific concordance was observed in a majority of cervical and LVPP pairs taken from women with initial and reappearing infections (71.4%). Taken together, these results suggest that it is unlikely that false positive detection or missed detection explained a majority of the recurrent detection episodes detected. It should be noted that in the immune competent host, reactivation is likely brought quickly under control by immune surveillance such that replicative infection and lesion development would be unlikely.
THE INFLUENCE OF STUDY DESIGN ON NATURAL HISTORY INFERENCE
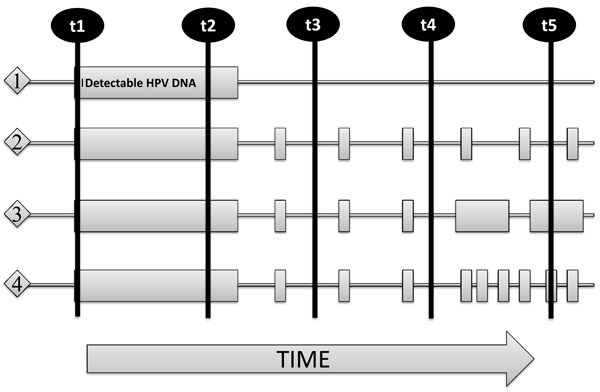
The results across these few studies which have directly measured recurrent detection of the same genotype show a wide range of cumulative probability of recurrence, and unfortunately offer little insight into the frequency or duration of recurrence. However, the study designs which rely on HPV DNA assessment at long intervals may be limiting our ability to accurately characterize the frequency and duration of recurrent detection. Fig. (1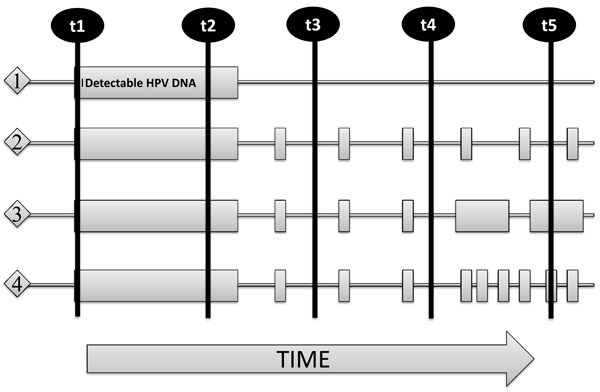 ) illustrates the limitations of the standard HPV natural history study designs on the characterization of HPV recurrent detection. Using these long interval sampling designs forces some important restrictions on the interpretation of natural history data.
) illustrates the limitations of the standard HPV natural history study designs on the characterization of HPV recurrent detection. Using these long interval sampling designs forces some important restrictions on the interpretation of natural history data.
The first is a problem of what epidemiologists refer to as 'left truncation' of data. This occurs when the natural history of an infection prior to study entry is unknown, as is the case for HPV. The result of this left truncation is that we cannot know, among all women entering the study negative for a specific HPV type, which ones had infection with that type in the past, and which ones did not. This has two implications in our study inferences. First, any newly detected HPV type among women entering the study negative for that type will be recorded and analyzed as an 'incident' infection. However, given the fact that we have demonstrated a non-negligible rate of new type-specific detection following a period of non-detection, we are likely misclassifying some unknown fraction of recurrent detection as 'incident'. These natural history designs thus not only are likely to underestimate the rate of recurrent detection, but overestimate the rate of 'incident' infection (i.e., acquisition).
The second problem is that of 'right truncation' of data, which occurs when we are unable to know the longer term natural history of an infection observed during our study after the observational period has ended. In the context of estimating recurrence rate in studies with anywhere from 2-10 years of follow-up, infections first observed to become undetectable late in the study have less opportunity to be observed to recur compared with infections first observed to become undetectable early in follow-up. These issues can be addressed using appropriate statistical methods, but the power of the study to estimate recurrence will be highly dependent on the total study duration.
A third problem particular to the issue of characterization of recurrence patterns in the long interval designs is essentially a combination of left and right truncation - that of the detection patterns of HPV in the unobserved time between study visits. The scarcity of data available to provide insight on HPV natural history over shorter time frames is a major limitation to an accurate understanding of the dynamic natural history of HPV. One study of high-risk adolescent girls (n=60, age 14-17 years) has shown that if samples are collected frequently (weekly), the patterns of detection of type-specific HPV are highly variable [10 Brown DR, Shew ML, Qadadri B, et al. A longitudinal study of genital human papillomavirus infection in a cohort of closely followed adolescent women J Infect Dis 2005; 191: 182-92.]. A comparison of the point prevalence at study entry and exit with cumulative prevalence across all study visits provides a good illustration of the potential bias in our estimates of HPV infection when using long interval sampled designs; 28.3% and 40.0% any HPV prevalence at entry and exit samples compared with 81.7% ever positive over the 2.2 years median follow-up. We have also observed patterns of short term HPV detection variability in a similar study of 33 monogamously sexually active adult women self-sampling twice per week for 3 menstrual cycles, and found the average duration of detection before return to negative was around 7 days, and we estimated that infection status based on a single swab would underestimate the 16-week cumulative prevalence of high-risk (HR) HPV by 56% (IQR -60.2%--48.8%) Su-Hsun Liu and Patti Gravitt, personal communication.
These data suggest that the 'true' duration of HPV infection is shorter than commonly reported. This is likely the case for the duration of 'detectable' HPV DNA. However, as Weaver, et al. have reported, re-analysis of "HPV negative" samples flanked by positive samples using highly sensitive PCR techniques identifies the presence of very low copies of viral DNA [11 Weaver B, Shew M, Qadadri B, et al. Low-level persistence of human papillomavirus 16 DNA in a cohort of closely followed adolescent women J Med Virol 2011; 83: 1362-9.]. In fact, total median duration of detectable HPV16 infection increased from 428 days (SD 852.5 days) using standard HPV Linear Array tests to 1,022.5 days (SD 943.7 days) using more sensitive type-specific nested PCR assays. Thus, it appears that standard epidemiologic study designs and HPV detection methods lead to both overestimation of the duration of detectable runs of HPV and to underestimation of the true duration of HPV carriage. Even after HPV DNA becomes undetectable using super sensitive nested PCR from exfoliated swab samples, the negative test result does not preclude the retention of a few quiescent HPV-infected cells in the basal stem cell pool. In this case, in the absence of microdissection and genotyping every basal epithelial stem cell, it would be impossible to prove eradication of infection.
THE ROLE OF HOST IMMUNITY IN HPV LATENCY AND REACTIVATION
Recently, Doorbar, et al. reported an increase in ROPV reactivation following immune suppression of latently infected rabbits [12 Doorbar J, Maglennon G, Hughes O, McIntosh P. Reactivation of latent papillomavirus genomes at sites of previous infection Basic Science Abstract Book. In: 27th International Papillomavirus Conference and Clinical Workshop; 2011 Sept 17-22; Berlin, Germany. p 59. Abstract nr O-25.01], suggesting a role for host immunity in suppressing viral reactivation. There are several studies suggesting a similar role of immune control of papillomavirus latency in humans. First, HPV-associated cancers are increased in patients with HIV-associated immune suppression and iatrogenic immune suppression following organ transplant [13 Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis Lancet 2007; 370(9581 ): 59-67.]. Few studies have evaluated the natural history of cervical HPV infection in transplant patients, but there is an abundance of data to show the effect of HIV-mediated immune suppression on the natural history of HPV infection. It has long been shown that HIV-infected women have both a higher incidence and a longer duration of HPV infection compared with HIV-uninfected women [8 Strickler HD, Burk RD, Fazzari M, et al. Natural history and possible reactivation of human papillomavirus in human immunodeficiency virus-positive women J Natl Cancer Inst 2005; 97: 577-86.]. Generally, persistence of infection was attributed to the immunosuppressive effects of HIV, but the higher rates of incident infection were attributable both to a loss of protective immunity against re-infection and a higher sexual risk profile in HIV-infected compared with HIV-uninfected women. However, recent data from two large natural history studies of HPV in HIV-infected women are strongly suggestive that HIV infection leads to loss of immunologic control of infection with more frequent reactivation of longer duration. Both the Womens Interagency HIV study (WIHS) and the HIV Epidemiology Research Study (HERS) are large prospective studies of HIV-infected and 'risk-matched' HIV-uninfected women which have evaluated cervical HPV outcomes over an extended follow-up interval. Table 2 summarizes evidence from each study supporting a critical role for T-cell mediated immunity in suppressing HPV reactivation. To determine the possible influence of HIV on HPV reactivation, Strickler, et al. compared the cumulative proportion of new HPV DNA detection among sexually active women and women with at least 18 consecutive months of sexual abstinence in the WIHS [8 Strickler HD, Burk RD, Fazzari M, et al. Natural history and possible reactivation of human papillomavirus in human immunodeficiency virus-positive women J Natl Cancer Inst 2005; 97: 577-86.]. The rate of new HPV DNA detection in sexually abstinent women without HIV infection was 5%, strikingly similar to the rate of recurrent type-specific detection observed in the studies in Table 1. The rates of new HPV DNA detection in the sexually abstinent HIV-infected women were higher, and increased as the CD4 T-cell count dropped, from 13% in the most immune competent to 22% in the most immune compromised HIV-infected women. Theiler, et al, went one step further by reporting recurrent detection of type-specific HPV DNA following a period of non-detection among women reporting no current sexual activity in the HERS [9 Theiler RN, Farr SL, Karon JM, et al. High-risk human papillomavirus reactivation in human immunodeficiency virus-infected women: risk factors for cervical viral shedding Obstet Gynecol 2010; 115: 1150-8.]. Rates of recurrent detection of HPV16 were 2.7/100 woman-years and 3.3/100 woman-years in sexually abstinent and sexually active women, respectively. Because women in both of these studies had similar baseline risks of past HPV infection (similar distribution of numbers of lifetime sex partners in WIHS and similar HPV seroprevalence in HERS) and by design removed any influence of unmeasured behavior of male sexual partners, the strong associations between new or recurrent HPV DNA detection and markers of immunity suggest a critical role for a competent T-cell immune memory in controlling HPV reactivation. Two studies evaluated HPV detection in periods before and after HIV acquisition and found that new HPV DNA detection increased rapidly (i.e., within weeks) following HIV-acquisition [14 Wang C, Wright TC, Denny L, Kuhn L. Rapid rise in detection of human papillomavirus (HPV) infection soon after incident HIV infection among South African women J Infect Dis 2011; 203(4 ): 479-86., 15 Nowak RG, Gravitt PE, Morrison CS, et al. Increases in human papillomavirus detection during early HIV infection among women in Zimbabwe J Infect Dis 2011; 203(8 ): 1182-91.]. Because HIV is known to rapidly obliterate the tissue-resident memory T-cell pool in the mucosal epithelium within weeks of infection [17 Mattapallil JJ, Douek DC, Hill B, Nishimura Y, Martin M, Roederer M. Massive infection and loss of memory CD4+T-cells in multiple tissues during acute SIV infection Nature 2005; 434(7037 ): 1093-7., 18 Veazey RS, Marx PA, Lackner AA. Vaginal CD4+ T cells express high levels of CCR5 and are rapidly depleted in simian immunodeficiency virus infection J Infect Dis 2003; 187: 769-.] the data from Wang and Nowak suggest more specifically that resident HPV-specific memory T-cells may be important in the control of HPV latency. Since activated memory T-cells contain the CCR-5 HIV co-receptor, a mechanism of HPV control through tissue resident memory T-cells may help to explain the recent reports of an increase in HIV acquisition among HPV positive women and men [16 Averbach SH, Gravitt PE, Nowak RG, et al. The association between cervical human papillomavirus infection and HIV acquisition among women in Zimbabwe AIDS 2010; 24(7 ): 1035-42., 19 Smith-McCune KK, Shiboski S, Chirenje MZ, et al. Type-specific cervico-vaginal human papillomavirus infection increases risk of HIV acquisition independent of other sexually transmitted infections PLoS One 2010; 5(4 ): e10094.-22 Chin-Hong PV, Husnik M, Cranston RD, et al. Anal human papillomavirus infection is associated with HIV acquisition in men who have sex with me AIDS 2009; 23(9 ): 1135-42.].
It is likely that more subtle, and possibly transient, forms of immune suppression also contribute to HPV reactivation. For example, a study of women over age 45 years in Guanacaste, Costa Rica reported that 21% of new HPV detection could be attributed to a reduced lymphoproliferative response to in vitro antigenic or mitogenic stimulation of PBMCs, and this was the only factor associated with new HPV detection among women who were not currently sexually active [23 Gonzalez P, Hildesheim A, Rodriguez AC, et al. Behavioral/lifestyle and immunologic factors associated with HPV infection among women older than 45 years Cancer Epidemiol Biomarkers Prev 2010; 19(12 ): 3044-54.]. We have shown that 85% of all newly detected HPV in women aged 35-60 years occurred in sexually abstinent or monogamous women, and that the population risk attributable to a higher number of lifetime sex partners was higher than that attributable to new sex partners in this population (PAR 71.7% and 13.0%, respectively) [24 Rositch AF, Burke AE, Viscidi RP, Silver MI, Chang K, Gravitt PE. Contributions of recent and past sexual partnerships on incident human papillomavirus detection: acquisition and reactivation in older women Cancer Res 2012 Sept 27; [Epub ahead of print]]. This data, in combination with studies showing an increase in HPV prevalence and incidence at older ages [25 Munoz N, Mendez F, Posso H, et al. Incidence, duration, and determinants of cervical human papillomavirus infection in a cohort of Colombian women with normal cytological results J Infect Dis 2004; 190(12 ): 2077-87.], suggest that the menopausal transition may represent a vulnerable window for immune suppression (possibly hormone-mediated) and HPV reactivation. In addition, the increased risk of HPV recurrence in patients with recurrent respiratory papillomatosis (RRP) [26 Chow LT, Broker TR, Steinberg BM. The natural history of human papillomavirus infections of the mucosal epithelia APMIS 2010; 118: 422-9.] and the higher prevalence of HPV and cervical neoplasia reported in women with autoimmune conditions such as lupus [27 Santana IU, Gomes Ado N, Lyrio LD, Rios Grassi MF, Santiago MB. Systemic lupus erythematosus, human papillomavirus infection, cervical pre-malignant and malignant lesions: a systematic review Clin Rheumatol 2011; 30(5 ): 665-72.], highlight additional populations who might contribute significantly to our understanding of the mechanisms of immune control of HPV infections.
IMPLICATIONS OF HPV LATENCY
Because the clinical and epidemiological communities have not systematically evaluated HPV latency, the clinical implications of a reactivated vs a recently acquired HPV infection are not clear. Certainly the increased risk of high grade neoplasia and cancer among HIV-infected and iatrogenically immune suppressed transplant recipients suggest that a reactivated infection carries a similar disease risk to a new infection. In addition, the high prevalence of high-risk (HR) HPV and low grade cytological abnormalities in these patients results in a high proportion of positive screening tests in the absence of detectable high-grade lesions [28 Harris TG, Burk RD, Palefsky JM, et al. Incidence of cervical squamous intraepithelial lesions associated with HIV serostatus, CD4 cell counts, and human papillomavirus test results JAMA 2005; 293(12 ): 1471-6.]. The resulting management of these frequently recurrent low grade lesions creates a burden and inefficiency of standard screening practices in these patient populations [29 Reimers LL, Sotardi S, Daniel D, et al. Outcomes after an excisional procedure for cervical intraepithelial neoplasia in HIV-infected women Gynecol Oncol 2010; 119(1 ): 92-7.].
Outside of the HIV and transplant populations, few other populations have been identified as being at high risk of reactivation. As reported earlier, there is mounting evidence that HPV reactivation, like other latent DNA infections, may increase at older ages. Many argue that the low prevalence of HR-HPV and cytological abnormalities in older women, as well as the plateau in incidence of invasive cervical cancer after age 55 [30 Plummer M, Peto J, Franceschi S. On behalf of the International Collaboration of Epidemiological Studies of Cervical Cancer. Time since first sexual intercourse and the risk of cervical cancer Int J Cancer 2012; 130: 2638-44.], suggest that even if HPV reactivates at older ages, there is minimal disease risk in the postmenopausal woman. However, we must remind the reader that reactivation risk will be directly proportionate to the total burden of past HPV infection. The populations of women in the United States and United Kingdom which contributed data to the older age groups until now all had sexual debut well before the sexual revolution that occurred from 1965-1975. Rates of sexually transmitted infections, including HPV, doubled during this time period. As such, the women we have observed during menopause to date were likely to have at least half the risk of HPV reactivation as women who are now entering menopause (because they were half as likely to ever be infected). Because of this cohort effect, we cannot rely on past epidemiological data or clinical observation from older women to predict the HPV and associated disease risk that will occur in the large population of women who will enter the menopausal transition in the next ten years with twice the lifetime HPV prevalence as previous generations. The possible impact is particularly troublesome given the well-documented problems associated with screening and diagnosis of HPV and associated lesions in the post-menopausal woman [31 Rositch AF, Silver MI, Burke A, et al. The correlation between HPV positivity and abnormal cervical cytology differs by age among perimenopausal women J Lower Genital Tract Dis 2012. [Epub ahead of print]-36 Stoler MJ, Wright TC Jr, Sharma A, et al. The interplay of age stratification and HPV testing on the predictive value of ASC-US cytology. Results from the ATHENA HPV study Am J Clin Pathol 2012; 137(2 ): 295-303.]. Acknowledging that reactivation might account for a higher proportion of new HPV detection in older women, investigators evaluated the risk of CIN2/3 in the Guanacaste cohort following new HPV detection in younger and older women [7 Rodriguez AC, Schiffman M, Herrero R, et al. Low risk of type-specific carcinogenic HPV re-appearance with subsequent cervical intraepithlelial neoplasia grade 2/3 Int J Cancer 2012; 131(8 ): 1874-81.]. They conclude that reactivation carries no unique risk compared with new infection. However, given the limitations of screening and diagnosis of pre-invasive lesions using standard screening algorithms, the risk of a higher proportion of undiagnosed lesions in the older population cannot be ruled out. Longer term follow-up with invasive cancer endpoints in this extensively followed population will be important to clarify the risk of cervical disease following HPV reactivation in older women.
In addition to the clinical implications of HPV latency, there are potentially important policy implications to continued disregard of the possibility of lifelong HPV infection as a latent infection at risk of reactivation. The development of cervical cancer screening and HPV vaccine policy and guidelines are guided by evidence-based review of the literature and mathematical prediction modeling. The issues raised in the section "The Influences of study design on HPV natural history inference" are most important in this context. Multiple parameter sets can provide a good fit to observed data, but inappropriate attribution of a model can lead to ineffective or possibly even harmful interventions. To this end, an unbiased evaluation of multiple possible models and collection of data to fill influential data gaps is prudent given the billions spent on global cervical cancer prevention.
SUMMARY
HPV and cervical cancer has served as a model for rapid and effective translation of research to practice. The interdisciplinary efforts that contributed to the success are arguably unparalleled. It is thus incredible that a consensus on whether HPV is a lifelong latent or transient infection has proven so elusive. In part, this can be attributed to the lack of molecular tools to definitively distinguish a latent from a recently acquired infection. We have faced similar methodologic challenges in the past - HPV is not readily culturable, it cannot infect other animals, and few other mammalian papillomaviruses infect and cause disease in the genital tract of their hosts. Despite these limitations, the research community relied heavily on overwhelming circumstantial evidence to move the field forward in the face of uncertainty. Understanding more clearly the longer term implications of HPV latency on a highly infected and aging population is of paramount importance, and the influence of latency and reactivation must take a central role in interpretation of both epidemiological and clinical observations moving forward.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
P. Gravitt supported by NIH NCI R01CA123467 and NIH NCI R21 CA156537.