- Home
- About Journals
-
Information for Authors/ReviewersEditorial Policies
Publication Fee
Publication Cycle - Process Flowchart
Online Manuscript Submission and Tracking System
Publishing Ethics and Rectitude
Authorship
Author Benefits
Reviewer Guidelines
Guest Editor Guidelines
Peer Review Workflow
Quick Track Option
Copyediting Services
Bentham Open Membership
Bentham Open Advisory Board
Archiving Policies
Fabricating and Stating False Information
Post Publication Discussions and Corrections
Editorial Management
Advertise With Us
Funding Agencies
Rate List
Kudos
General FAQs
Special Fee Waivers and Discounts
- Contact
- Help
- About Us
- Search

The Open Nutrition Journal
(Discontinued)
ISSN: 1874-2882 ― Volume 15, 2021
Effect of Oral Nutritional Supplementation on Growth in Vietnamese Children with Stunting
Dung T. Pham1, *, Trong N. Hoang1, Nhu T. Ngo1, Long H. Nguyen2, Trung Q. Tran2, Hanh M. Pham1, Dieu T. T. Huynh3, Nhung T. Ninh1
Abstract
Background:
The impact of oral nutritional supplementations (ONS) is not well-elucidated in children with stunting.
Objective:
The aim is to evaluate the effect of ONS on growth in Vietnamese children with stunting.
Methods:
This 6-month, prospective, single-arm trial evaluated 121 children aged 24–48 months with stunting (height-for-age z-score [HAZ] < -2) and low weight-for-height z-score (WHZ < -1) in Vietnam. Children consumed ONS twice daily. The outcomes included the change in HAZ, WHZ, and weight-for-age z-score (WAZ) from baseline to 3- and 6 months; change in height and weight from baseline to 3- and 6 months; and the prevalence of stunting, wasting (WHZ < -2 SD), and underweight (WAZ < -2 SD) at 6 months. We also examined factors associated with a change in HAZ over the intervention period.
Results:
The mean age was 34.7 months and 49% were male. Height and weight increased from baseline to 3- and 6-months (p<0.0001). There was a significant increase in median HAZ (0.25 units), WHZ (0.72 units), and WAZ (0.65 units) from baseline to 6 months (p<0.0001). Notably, approximately 40% of children recovered from stunting at 6 months (p<0.0001). The prevalence of wasting and underweight status were also significantly lower at 6 months (p=0.0310 and p<0.0001, respectively) relative to the baseline. Lower HAZ and younger age at baseline were significantly associated with higher linear growth at 6 months.
Conclusion:
ONS helped improve linear and ponderal growth and reduce the prevalence of stunting, wasting, and underweight status in stunted children at risk of wasting.
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 43
Last Page: 52
Publisher Id: TONUTRJ-13-43
DOI: 10.2174/1874288201913010043
Article History:
Received Date: 10/06/2019Revision Received Date: 30/09/2019
Acceptance Date: 02/10/2019
Electronic publication date: 11/12/2019
Collection year: 2019
open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
* Address correspondence to this author at the Thai Binh University of Medicine and Pharmacy Nutrition and Food Safety Department, No. 373, Ly Bon Street, Thai Binh city, Thai Binh province, 410000, Vietnam; Tel: 84 989981359;
Fax: 84 2273 847509; E-mail: dungpt@tbmc.edu.vn
| Open Peer Review Details | |||
|---|---|---|---|
| Manuscript submitted on 10-06-2019 |
Original Manuscript | Effect of Oral Nutritional Supplementation on Growth in Vietnamese Children with Stunting | |
1. INTRODUCTION
Globally, stunting affected 151 million children under the age of 5 in 2017, with more than half of these children living in Asia [1UNICEF, WHO, World Bank Group. Levels and trends in child malnutrition 2018.https://www.who.int/nutgrowthdb/2018-jme-brochure.pdf?ua=1]. In Vietnam, nearly 1 in 4 children under the age of 5
are stunted [1UNICEF, WHO, World Bank Group. Levels and trends in child malnutrition 2018.https://www.who.int/nutgrowthdb/2018-jme-brochure.pdf?ua=1]. A child is considered to be stunted if his/her height-for-age falls more than 2 standard deviations (SDs) or z-scores are below the World Health Organization (WHO) Child Growth Standards mean for the same age and sex [2WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 2006; 450(Suppl. 450): 76-85.
[PMID: 16817681] ]. In Vietnam, child feeding practices, food insecurity (inability to obtain sufficient healthy food), and sub-optimal dietary diversity contribute to stunting [3Report GN. Global Nutrition Report. 2017 Global Nutrition Report. 2017 [cited 2018 Dec 13]. Available from:
https://globalnutritionreport .org/reports/2017-global-nutrition-report/-7Nguyen PH, Menon P, Ruel M, Hajeebhoy N. A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pac J Clin Nutr 2011; 20(3): 359-74.
[PMID: 21859654] ].
Stunted linear growth is a major indicator of childhood undernutrition as it leads to extensive health and socio-economic consequences, including increased mortality and morbidity from infectious diseases as well as impaired cognitive, psychological and behavioral development in childhood and adolescence [8Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013; 382(9890): 427-51.
[http://dx.doi.org/10.1016/S0140-6736(13)60937-X] [PMID: 23746772] -12Walker SP, Chang SM, Powell CA, Simonoff E, Grantham-McGregor SM. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation. J Nutr 2007; 137(11): 2464-9.
[http://dx.doi.org/10.1093/jn/137.11.2464] [PMID: 17951486] ]. In the long-term, stunting contributes to shorter adult height, lower attained schooling, reduced income and productivity, decreased offspring birth weight, and increased risk for the development of chronic disease [13Adair LS, Fall CH, Osmond C, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet 2013; 382(9891): 525-34.
[http://dx.doi.org/10.1016/S0140-6736(13)60103-8] [PMID: 23541370] -16Martorell R, Horta BL, Adair LS, et al. Weight gain in the first two years of life is an important predictor of schooling outcomes in pooled analyses from five birth cohorts from low- and middle-income countries. J Nutr 2010; 140(2): 348-54.
[http://dx.doi.org/10.3945/jn.109.112300] [PMID: 20007336] ].
Nutritional interventions for stunting aim to improve nutritional intake and provide all essential nutrients that are required to promote catch-up growth. To overcome stunting, energy intake must be optimized in conjunction with the intake of macronutrients, such as protein, and micronutrients, including zinc and vitamin A [17Golden MH. Proposed recommended nutrient densities for moderately malnourished children. Food Nutr Bull 2009; 30(3)(Suppl.): S267-342.
[http://dx.doi.org/10.1177/15648265090303S302] [PMID: 19998863] -20Marriott BP, White A, Hadden L, Davies JC, Wallingford JC. World Health Organization (WHO) infant and young child feeding indicators: associations with growth measures in 14 low-income countries. Matern Child Nutr 2012; 8(3): 354-70.
[http://dx.doi.org/10.1111/j.1740-8709.2011.00380.x] [PMID: 22171937] ]. Dietary counseling (DC) using family foods is one such strategy for addressing child malnutrition [21Ashworth A, Ferguson E. Dietary counseling in the management of moderate malnourishment in children. Food Nutr Bull 2009; 30(3)(Suppl.): S405-33.
[http://dx.doi.org/10.1177/15648265090303S304] [PMID: 19998865] , 22Bhutta ZA, Ahmed T, Black RE, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet 2008; 371(9610): 417-40.
[http://dx.doi.org/10.1016/S0140-6736(07)61693-6] [PMID: 18206226] ]. However, several challenges may limit the effectiveness of a food-based approach in developing countries [23de Pee S, Bloem MW. Current and potential role of specially formulated foods and food supplements for preventing malnutrition among 6- to 23-month-old children and for treating moderate malnutrition among 6- to 59-month-old children. Food Nutr Bull 2009; 30(3)(Suppl.): S434-63.
[http://dx.doi.org/10.1177/15648265090303S305] [PMID: 19998866] ]. In Vietnam, family foods typically comprise of rice, legumes, oilseeds, vegetables, sugar, salt, and monosodium glutamate, which have high antinutrient content and low density in terms of macro- and micronutrients [7Nguyen PH, Menon P, Ruel M, Hajeebhoy N. A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pac J Clin Nutr 2011; 20(3): 359-74.
[PMID: 21859654] , 18Michaelsen KF, Hoppe C, Roos N, et al. Choice of foods and ingredients for moderately malnourished children 6 months to 5 years of age. Food Nutr Bull 2009; 30(3)(Suppl.): S343-404.
[http://dx.doi.org/10.1177/15648265090303S303] [PMID: 19998864] , 24Pham VP, Nguyen VH, Salvignol B, et al. A six-month intervention with two different types of micronutrient-fortified complementary foods had distinct short- and long-term effects on linear and ponderal growth of Vietnamese infants. J Nutr 2012; 142(9): 1735-40.
[http://dx.doi.org/10.3945/jn.111.154211] [PMID: 22810985] ]. Furthermore, there is poor consumption of fruits, fish, and animal-based foods in Vietnam [7Nguyen PH, Menon P, Ruel M, Hajeebhoy N. A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pac J Clin Nutr 2011; 20(3): 359-74.
[PMID: 21859654] ]. Another challenge of using DC to overcome stunting is that it requires dietary diversity [20Marriott BP, White A, Hadden L, Davies JC, Wallingford JC. World Health Organization (WHO) infant and young child feeding indicators: associations with growth measures in 14 low-income countries. Matern Child Nutr 2012; 8(3): 354-70.
[http://dx.doi.org/10.1111/j.1740-8709.2011.00380.x] [PMID: 22171937] ] and may be difficult to implement considering the aforementioned issues related to food insecurity and diversity in Vietnam. Moreover, dietary recommendations for moderately stunted children are non-specific and this may limit their effectiveness for catch-up growth [21Ashworth A, Ferguson E. Dietary counseling in the management of moderate malnourishment in children. Food Nutr Bull 2009; 30(3)(Suppl.): S405-33.
[http://dx.doi.org/10.1177/15648265090303S304] [PMID: 19998865] ].
Other strategies for addressing stunting have varying success. For example, fortified blended foods (corn-soy or wheat-soy blends) contain antinutrients, have inadequate micronutrients, and are deficient in milk [23de Pee S, Bloem MW. Current and potential role of specially formulated foods and food supplements for preventing malnutrition among 6- to 23-month-old children and for treating moderate malnutrition among 6- to 59-month-old children. Food Nutr Bull 2009; 30(3)(Suppl.): S434-63.
[http://dx.doi.org/10.1177/15648265090303S305] [PMID: 19998866] , 25Fleige LE, Moore WR, Garlick PJ, et al. Recommendations for optimization of fortified and blended food aid products from the United States. Nutr Rev 2010; 68(5): 290-315.
[http://dx.doi.org/10.1111/j.1753-4887.2010.00288.x] [PMID: 20500790] ]. Additionally, supplementation with type II nutrients (protein and zinc, in particular) may positively affect linear growth while there is varying evidence on the impact of micronutrient supplementation on height [19Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36.
[http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] , 26Salam RA, MacPhail C, Das JK, Bhutta ZA. Effectiveness of Micronutrient Powders (MNP) in women and children. BMC Public Health 2013; 13(Suppl. 3): S22.
[PMID: 24564207] -30Millward DJ. Nutrition, infection and stunting: the roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children. Nutr Res Rev 2017; 30(1): 50-72.
[http://dx.doi.org/10.1017/S0954422416000238] [PMID: 28112064] ]. Recent studies have also investigated small-quantity lipid-based nutrient supplements (LNS), a type of home fortification that delivers energy, protein, essential fatty acids and micronutrients in a food base, for overcoming undernutrition in infants. However, results with LNS have been variable as they do not seem to promote linear growth in all infant populations [30Millward DJ. Nutrition, infection and stunting: the roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children. Nutr Res Rev 2017; 30(1): 50-72.
[http://dx.doi.org/10.1017/S0954422416000238] [PMID: 28112064] -33Adu-Afarwuah S, Lartey A, Okronipa H, et al. Small-quantity, lipid-based nutrient supplements provided to women during pregnancy and 6 mo postpartum and to their infants from 6 mo of age increase the mean attained length of 18-mo-old children in semi-urban Ghana: a randomized controlled trial. Am J Clin Nutr 2016; 104(3): 797-808.
[http://dx.doi.org/10.3945/ajcn.116.134692] [PMID: 27534634] ].
In this milieu, oral nutritional supplements (ONS), which are specially formulated to provide energy, macronutrients and micronutrients, have been shown to be effective for linear growth. In a randomized controlled trial (RCT) in preschool children with picky eating behavior and growth faltering (weight-for-height percentile <25th percentile), the provision of ONS and DC for 3 months resulted in significant increases in weight-for-height, weight-for-age, and height-for-age percentiles compared with DC alone. ONS also significantly reduced the incidence of upper respiratory tract infections in these children [34Alarcon PA, Lin LH, Noche M Jr, et al. Effect of oral supplementation on catch-up growth in picky eaters. Clin Pediatr (Phila) 2003; 42(3): 209-17.
[http://dx.doi.org/10.1177/000992280304200304] [PMID: 12739919] ]. Additionally, long-term intervention with ONS plus initial DC promoted longitudinal ponderal and linear growth in nutritionally-at risk children aged 36–48 months [35Huynh DT, Estorninos E, Capeding RZ, Oliver JS, Low YL, Rosales FJ. Longitudinal growth and health outcomes in nutritionally at-risk children who received long-term nutritional intervention. J Hum Nutr Diet 2015; 28(6): 623-35.
[http://dx.doi.org/10.1111/jhn.12306] [PMID: 25808062] ]. Long-term ONS with initial DC was also associated with improved dietary diversity as well as adequate dietary intake of nutrients over 48 weeks and did not interfere with the intake of family foods [36Huynh DT, Estorninos E, Capeding MR, Oliver JS, Low YL, Rosales FJ. Impact of long-term use of oral nutritional supplement on nutritional adequacy, dietary diversity, food intake and growth of Filipino preschool children. J Nutr Sci 2016; 5: e20.
[http://dx.doi.org/10.1017/jns.2016.6] [PMID: 27293557] ]. Even in the absence of DC, ONS improved height and weight in short and lean prepubertal healthy children, who did not frequently consume a well-balanced diet [37Lebenthal Y, Yackobovitch-Gavan M, Lazar L, et al. Effect of a nutritional supplement on growth in short and lean prepubertal children: a prospective, randomized, double-blind, placebo-controlled study. J Pediatr 2014; 165(6): 1190-1193.e1.
[http://dx.doi.org/10.1016/j.jpeds.2014.08.011] [PMID: 25241181] ].
While the benefits of short-term and long-term interventions with ONS for growth are well-established, the impact of ONS on physical growth in children with stunting is less clearly defined. In this context, we examined the efficacy of ONS on linear and ponderal growth in preschool children with stunting (height-for-age z-score [HAZ] < -2) and low weight-for-height z-score (WHZ < -1) in Vietnam.
2. MATERIALS AND METHODS
2.1. Study Design and Participants
We conducted a prospective, single-arm intervention study in Thai Binh province, Vietnam between September 2015 and June 2016. Children were recruited from a nutritional screening program in two preschools in the Tien Hai district of Thai Binh. Children attending these preschools were eligible for nutritional screening if they were 24–48 months of age at the time of screening and if their family provided consent for participating in the study. Based on the nutritional screening, children were eligible for inclusion in the study if they were 24–48 months old, had stunting (HAZ < -2), and were at nutritional risk (WHZ < -1). Children who had chronic diseases other than stunting, such as congenital malformation or severe acute illness, at the time of enrollment were excluded from the study.
The study was conducted in accordance with the ethical principles that have their origins in the Declaration of Helsinki. Written informed consent was obtained from each child’s parents or legal guardian. The study protocol and relevant documentation were approved by the Institutional Review Board of the Thai Binh University of Medicine and Pharmacy.
2.2. Intervention
Eligible children received two servings of ONS every day for 6 months. The commercially available ONS (PediaSure®; Abbott Laboratories, Vietnam) provides 450 kcal, 13.5g protein, and ≥50% micronutrient requirements when taken twice daily. Study collaborators trained preschool teachers and mothers to prepare the ONS according to the label instructions. Under the teachers’ supervision, children consumed the ONS in the classroom at snack times (i.e. between main meals) in the morning and the afternoon during 6 days of the week. Parents were instructed to provide ONS to the child on Sunday when children did not attend school.
2.3. Outcome Assessments
The primary outcome was the change in HAZ from baseline to 6 months of intervention. Other outcomes included the change in weight-for-age z-score (WAZ) and WHZ from baseline to 3- and 6 months and the change in weight and height from the baseline to 3 months and 6 months. Height-for-age, weight-for-age, and weight-for-height were calculated as sex-age-specific z-scores based on the WHO Child Growth Standards [2WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 2006; 450(Suppl. 450): 76-85.
[PMID: 16817681] ]. Stunting was defined as HAZ < -2 SD, underweight was defined as WAZ < -2 SD, and wasting was defined as WHZ < -2 SD.
Additionally, we analyzed the prevalence of stunting, underweight, and wasting status at baseline and 6 months. We also examined the effects of several factors, including age, sex, baseline HAZ, and parental education on change in HAZ over the 6-month study period. Reports of adverse events (AEs) and serious AEs were collected over the study period.
2.4. Anthropometric Assessment
Anthropometric measurements were performed by research staff from the Nutrition and Food Safety Department of the Thai Binh University of Medicine and Pharmacy who were trained on standardized methods of conducting these measurements. Body weight was measured with light clothes and without shoes and jackets using an electronic weighing scale (Tanita Limited, Itabashi-Ku, Tokyo Japan) and recorded to the nearest 0.1 kg. Standing height was measured without shoes or hat using a portable measuring board provided by the National Institution of Nutrition, Vietnam and recorded to the nearest 0.1 cm. Weight and height were measured at baseline and at 3 and 6 months.
2.5. Compliance Assessment
Compliance with the ONS was assessed from the product intake records that teachers completed on a daily basis on the weekdays. Parents reported their child’s intake during the weekend using these records. Compliance with the ONS was determined by calculating the percentage of actual product consumed. This percentage was obtained by dividing the number of servings that were consumed by the number of servings that were instructed to be consumed over the 6 month period.
2.6. Statistical Analyses
The sample size was estimated using the Hazard formula. A minimum sample size of 120 children was required to provide 90% power to detect a difference of 0.15 and 0.25 SD in the mean change in HAZ from baseline to 6 months. Based on an estimated attrition rate of 20% (24 children), 144 children needed to enroll in this study for adequate power.
All statistical analyses were performed on an evaluable analysis, using SAS version 9.04. Descriptive results, such as anthropometric measurements, were summarized by the mean, and SD or median and the interquartile range (IQR). Categorical variables were summarized by the number of subjects (n) and as a percentage (%). All continuous variables were checked for normality using Skewness and Kurtosis tests. Nonparametric tests, such as the Mann–Whitney U-test and the Wilcoxon signed-rank tests, were used to examine differences between two groups for continuous variables with non-normal distribution. Mixed-effect models were used to estimate the mean HAZ, WAZ, and WHZ over the study period, after adjustment for confounding factors such as the child’s age, sex, baseline HAZ and parental education level. The McNemar’s test was used to compare the prevalence of stunting, underweight and wasting at baseline and at 6 months of intervention. The Proc mixed procedure, controlled for confounding factors, was used to calculate the significance of factors associated with the change in HAZ over the 6-month study period.
3. RESULTS
3.1. Study Participants
Of the 800 children who underwent nutritional screening in 3 villages in the Tien Hai District, 140 were enrolled in this study. Of the 140 enrolled children, 19 did not complete the study due to the loss to follow-up or change of residence or missed study procedures. 121 children were, therefore, remained included in the evaluable population-based on treatment compliance and data completeness.
Table 1 shows the baseline characteristics of children in the intent-to-treat population and their parents. The mean child age was 34.7 months and 49% were male. At baseline, males were heavier than females (p=0.002) while the mean height was similar between the sexes. Additionally, males had significantly higher HAZ (p=0.018) and lower WHZ (p=0.005) than females. WAZ was comparable between the sexes. With respect to parental characteristics, over 60% of mothers were educated up to a high school and/or university level.
3.2. Change in Anthropometric Indices Over Time
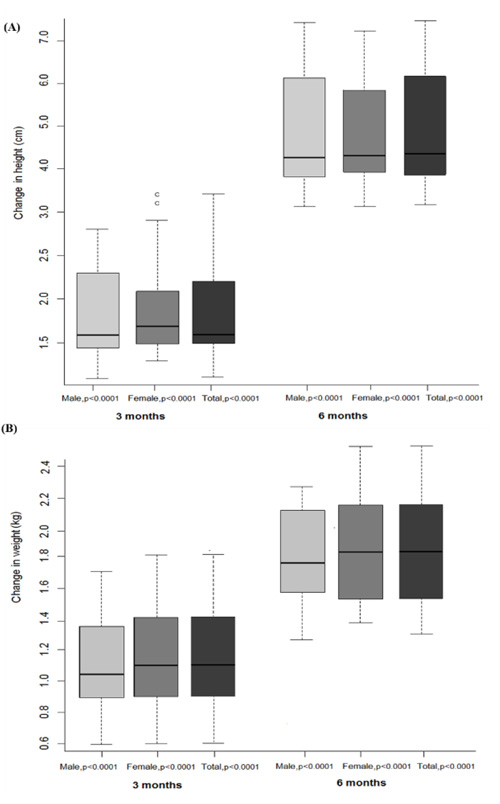
We assessed longitudinal growth using anthropometric indices measuring linear and ponderal growth over time. Fig. (1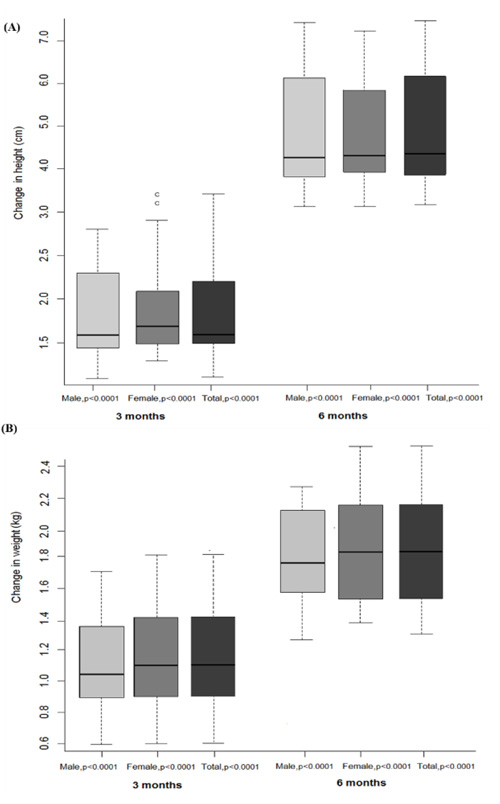 ) shows the median change in height and weight of the examined population from baseline to 3 months and 6 months of intervention. There were significant height and weight gain from baseline to 3 months and 6 months; the increase in these parameters was similar across sexes (p<0.0001; Fig. (1
) shows the median change in height and weight of the examined population from baseline to 3 months and 6 months of intervention. There were significant height and weight gain from baseline to 3 months and 6 months; the increase in these parameters was similar across sexes (p<0.0001; Fig. (1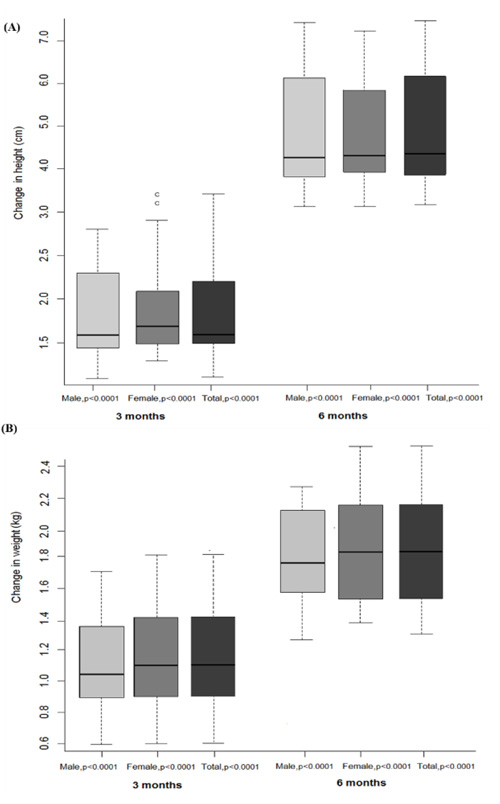 )). There was more height gain during the last 3 months of the intervention period (median change of 4.43 cm at 6 months; IQR3.9–6.2 cm) compared with the first 3 months (median change of 1.62 cm at 3 months; IQR 1.52–2.25 cm (Fig. 1a
)). There was more height gain during the last 3 months of the intervention period (median change of 4.43 cm at 6 months; IQR3.9–6.2 cm) compared with the first 3 months (median change of 1.62 cm at 3 months; IQR 1.52–2.25 cm (Fig. 1a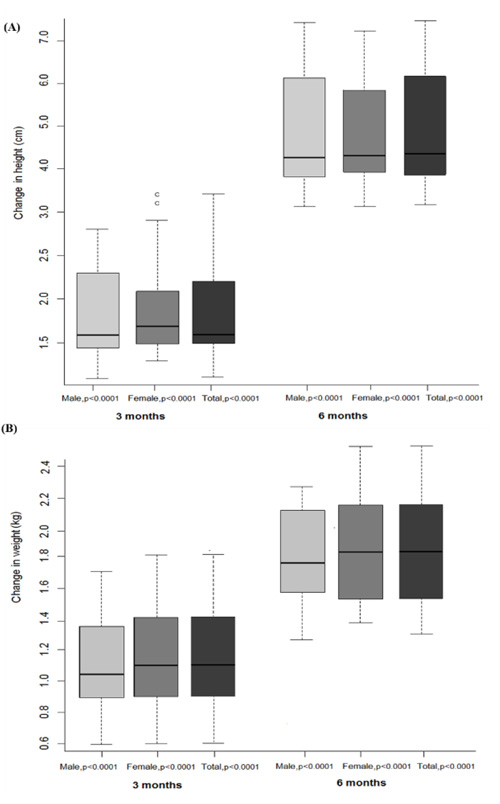 ). In contrast, weight steadily increased from baseline to 3 months (median change of 1.11 kg; IQR 0.91–1.40 kg) and 6 months (median change of 1.81 kg; IQR: 1.41–2.21 kg) (Fig. 1b
). In contrast, weight steadily increased from baseline to 3 months (median change of 1.11 kg; IQR 0.91–1.40 kg) and 6 months (median change of 1.81 kg; IQR: 1.41–2.21 kg) (Fig. 1b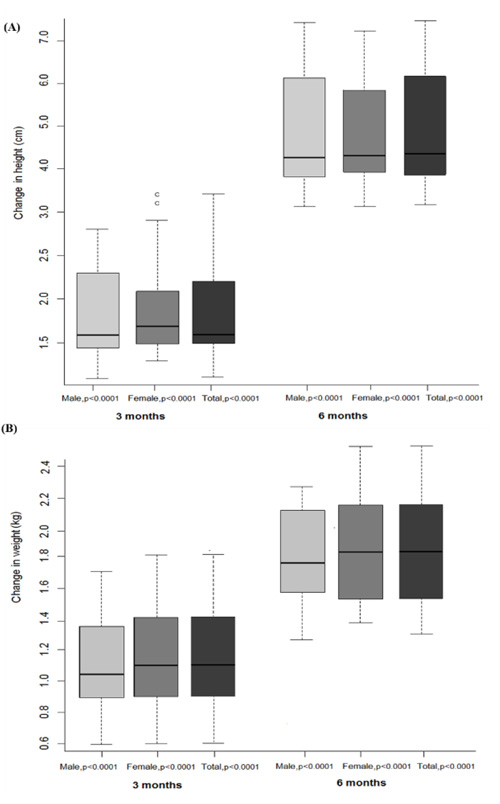 ).
).
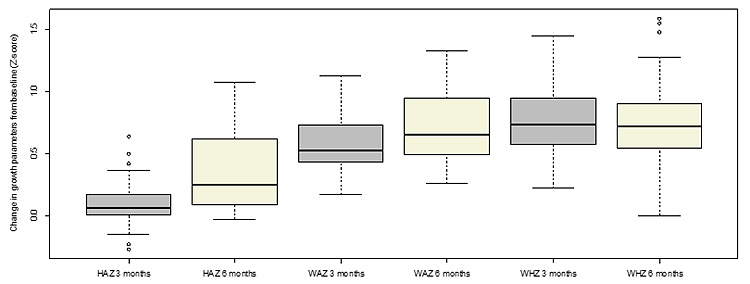
Fig. (2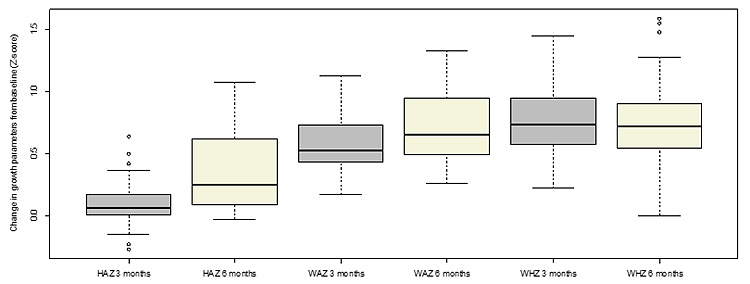 ) depicts the growth outcomes of the examined population expressed using the WHO Child Growth Standards. In terms of linear growth, there was a significant increase in the median HAZ from baseline to 3 months (p<0.0001) and 6 months of intervention (p<0.0001). At 6 months, children receiving the ONS had a 0.25 (IQR 0.09 to 0.623) z-score catch-up in median HAZ. There was also a significant improvement in ponderal growth as WAZ and WHZ significantly increased after 3 months (p<0.0001 for WAZ and WHZ) and 6 months of treatment with the ONS (p<0.0001). As was the case with the median HAZ, the median WAZ and WHZ shifted towards the normal distribution (0 z-score), which represents the reference population of the WHO Child Growth Standards, over the study period. At 6 months, the median WAZ improved by 0.65 units and the median WHZ improved by 0.72 units.
) depicts the growth outcomes of the examined population expressed using the WHO Child Growth Standards. In terms of linear growth, there was a significant increase in the median HAZ from baseline to 3 months (p<0.0001) and 6 months of intervention (p<0.0001). At 6 months, children receiving the ONS had a 0.25 (IQR 0.09 to 0.623) z-score catch-up in median HAZ. There was also a significant improvement in ponderal growth as WAZ and WHZ significantly increased after 3 months (p<0.0001 for WAZ and WHZ) and 6 months of treatment with the ONS (p<0.0001). As was the case with the median HAZ, the median WAZ and WHZ shifted towards the normal distribution (0 z-score), which represents the reference population of the WHO Child Growth Standards, over the study period. At 6 months, the median WAZ improved by 0.65 units and the median WHZ improved by 0.72 units.
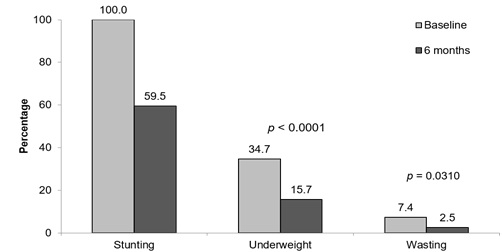 |
Fig. (3) Stunting, underweight and wasting status at baseline and 6 months. p-value is from McNemar’s test. |
3.3. Prevalence of Stunting, Underweight, and Wasting Status
Fig. (3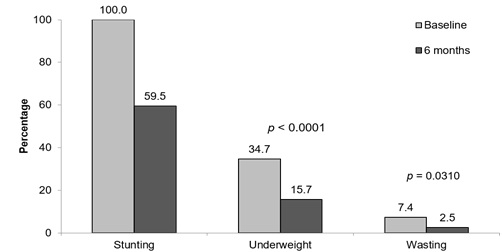 ) shows the magnitude of stunting (HAZ < -2), underweight (WAZ < -2) and wasting (WHZ < -2) at baseline and 6 months of intervention with ONS in the examined population. There was a significant decrease in the prevalence of stunting at 6 months of intervention when approximately 40% of children recovered from stunting based on the HAZ (p<0.0001). Additionally, relative to baseline rates, the prevalence of underweight (p<0.0001) and wasting status (p=0.0310) were also significantly reduced at 6 months.
) shows the magnitude of stunting (HAZ < -2), underweight (WAZ < -2) and wasting (WHZ < -2) at baseline and 6 months of intervention with ONS in the examined population. There was a significant decrease in the prevalence of stunting at 6 months of intervention when approximately 40% of children recovered from stunting based on the HAZ (p<0.0001). Additionally, relative to baseline rates, the prevalence of underweight (p<0.0001) and wasting status (p=0.0310) were also significantly reduced at 6 months.
3.4. Factors Associated with a Change in HAZ Over 6 Months
Factors associated with a change in HAZ over the study period are shown in Table 2. Over the 6 months, there was a significant increase in the HAZ of 0.06 units per month (p<0.0001). Additionally, baseline age and baseline HAZ were significantly associated with HAZ alteration, since young children displayed a greater increase in HAZ compared with older children. Each additional month of age was associated with a lower HAZ by 0.06 units at the end of the 6-month intervention (p<0.0001). Children who had 1.0-unit lower baseline HAZ had a small but significant increase in HAZ, resulting in smaller differences in their HAZ at 6 months with 0.94 units (p<0.001). In contrast, there was no association between sex and change in HAZ after 6 months of intervention. Similarly, parental education did not significantly affect the change in HAZ.
3.5. Compliance and Safety
All children in the examined population were reported to consume 75% of the recommended dose of the ONS on a daily basis. No AEs related to product consumption, including nausea, regurgitation, vomiting, flatulence, constipation or diarrhea, were reported during the intervention period.
4. DISCUSSION
In this study, we demonstrate that 6-month supplementation with ONS significantly improved linear and ponderal growth in preschool children with stunting and low WHZ. Additionally, ONS significantly reduced the prevalence of stunting as well as underweight and wasting status over the follow-up period.
Stunting is a dynamic process that reflects persistent or long-term malnutrition [17Golden MH. Proposed recommended nutrient densities for moderately malnourished children. Food Nutr Bull 2009; 30(3)(Suppl.): S267-342.
[http://dx.doi.org/10.1177/15648265090303S302] [PMID: 19998863] ]. Reversing stunting requires accelerated or catch-up growth, which is a growth in height above the normal rate for an age that occurs after a period of growth retardation [38Bhutta Z, Yackobovitch-Gavan M. Malnutrition and Catch-Up Growth during Childhood and Puberty. World Rev Nutr Diet 2016; 114: 120-7.
[http://dx.doi.org/10.1159/000441823] [PMID: 26914906] ]. Unlike weight gain, which requires higher energy intake, catch-up linear growth requires increased energy as well as growth and functional nutrients in adequate amounts for the synthesis of skeletal and lean tissue [17Golden MH. Proposed recommended nutrient densities for moderately malnourished children. Food Nutr Bull 2009; 30(3)(Suppl.): S267-342.
[http://dx.doi.org/10.1177/15648265090303S302] [PMID: 19998863] , 18Michaelsen KF, Hoppe C, Roos N, et al. Choice of foods and ingredients for moderately malnourished children 6 months to 5 years of age. Food Nutr Bull 2009; 30(3)(Suppl.): S343-404.
[http://dx.doi.org/10.1177/15648265090303S303] [PMID: 19998864] ]. The ONS used in this study was composed of high-quality protein, easily-digested fat, carbohydrates, and all the essential micronutrients that are necessary for growth and physiological functions. The applied ONS provided 33% of the energy and approximately 50% of the recommended daily micronutrient and protein requirements for Vietnamese children aged 3-5 years. Therefore, the significant benefits of ONS observed in our study support the vital role of multiple nutrient intervention approaches using energy, macronutrients and micronutrients in reversing stunting.
In the present study, treatment of stunted children with ONS for 6 months significantly improved HAZ by 0.25 units, WHZ by 0.72 units, and WAZ by 0.65 units from baseline. Other studies have also shown significant improvements in linear and ponderal growth in non-stunted children after intervention with ONS [34Alarcon PA, Lin LH, Noche M Jr, et al. Effect of oral supplementation on catch-up growth in picky eaters. Clin Pediatr (Phila) 2003; 42(3): 209-17.
[http://dx.doi.org/10.1177/000992280304200304] [PMID: 12739919] , 35Huynh DT, Estorninos E, Capeding RZ, Oliver JS, Low YL, Rosales FJ. Longitudinal growth and health outcomes in nutritionally at-risk children who received long-term nutritional intervention. J Hum Nutr Diet 2015; 28(6): 623-35.
[http://dx.doi.org/10.1111/jhn.12306] [PMID: 25808062] ]. However, in some studies that used similar ONS in non-stunted children, there was no significant improvement in HAZ after ONS application, although there was a trend towards the improved height and HAZ in the intervention groups [39Sheng X, Tong M, Zhao D, et al. Randomized controlled trial to compare growth parameters and nutrient adequacy in children with picky eating behaviors who received nutritional counseling with or without an oral nutritional supplement. Nutr Metab Insights 2014; 7: 85-94.
[http://dx.doi.org/10.4137/NMI.S15097] [PMID: 25342910] , 40Ghosh AK, Kishore B, Shaikh I, et al. Effect of oral nutritional supplementation on growth and recurrent upper respiratory tract infections in picky eating children at nutritional risk: a randomized, controlled trial. J Int Med Res 2018; 46(6): 2186-201.
[http://dx.doi.org/10.1177/0300060518757355] [PMID: 29614897] ]. This discrepancy may be attributed to the short study duration (3–4 months), the difference in supplementation dosage, the degree of growth deficits, and whether the children receiving the ONS had acute illnesses, such as upper respiratory tract infections, at baseline. In our study, compared with the normal rate of height gain based on the WHO Child Growth Standards at the median values for height-for-age, catch-up growth in height was more evident during the last 3 months of ONS intervention (1.4 times the normal rate) versus the initial 3 months (0.9 times). In contrast, compared with the normal rate of weight gain, the rate of weight gain in the present study was faster during the first 3 months (1.8 times) of treatment with ONS than the last 3 months (1.2 times).
Similar to the growth improvements with ONS in our study, several RCTs have demonstrated the impact of supplementary feeding interventions in children with stunting. Relative to controls, provision of micronutrient-fortified milk for 1 year significantly improved mean HAZ (0.28 unit increase from baseline), WAZ (0.38 unit increase), and WHZ (0.42 unit increase) in children aged 1–4 years, of whom nearly two-thirds were either stunted or stunted and wasted [41Sazawal S, Dhingra U, Dhingra P, et al. Micronutrient fortified milk improves iron status, anemia and growth among children 1-4 years: a double masked, randomized, controlled trial. PLoS One 2010; 5(8): e12167.
[http://dx.doi.org/10.1371/journal.pone.0012167] [PMID: 20730057] ]. Additionally, in an RCT involving children aged 25–48 months in the Thai Binh province, 12-month consumption of locally-available clam meat significantly improved mean HAZ (0.44 unit increase) relative to controls; stunting was reduced by 39% in children with stunting, who comprised 34% of the intervention group [42Tran TQ. Prevalence of stunting and the effects of consumption of a locally available seafood in improving stunting in children under 5 years old in Tien Hai, a coastal area of Thai Binh province, Vietnam. Thai Binh University of Medicine and Pharmacy, Vietnam 2014 Unpublished study ]. Comparatively, the ONS in our study resulted in a HAZ increase of 0.25 units, with similar levels of recovery from stunting (40%) after only 6 months of intervention. Another community-based RCT in 12–23-month-old Vietnamese children with stunting demonstrated that compared with DC alone, DC plus supplementary feeding using locally available foods significantly improves HAZ (0.60 unit increase) and stunting as 55% of the tested population was not classified as stunted at the end of the 12-month intervention period [43Nguyen VA, Le HT, Pham HTT, Doan HTT. Effect of supplementary feeding using locally available foods on improving stunting, Tien Lu district, Hung Yen Province. Vietnam Journal of Practical Medicine 2017; 1033: 35-9.]. The increase in HAZ reported by Vu et al. is higher than the HAZ increase (0.25 units) in our study, possibly because the children in the study by Vu et al. were younger than that participated in our study and may have experienced a greater increase in HAZ due to their younger age. Additionally, while 55% of children in the study by Vu et al. recovered from stunting after 1 year of intervention, 40% of the children in our sample recovered from stunting after only 6 months of intervention with ONS. A Cochrane meta-analysis of RCTs that included a wide age range (3 months–5 years) of children demonstrated a small but significant effect of supplementary feeding with food and/or drink on WAZ and HAZ while WHZ was not affected [44Kristjansson E, Francis DK, Liberato S, et al. Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years. Cochrane Database Syst Rev 2015; 3(3): CD009924.
[http://dx.doi.org/10.1002/14651858.CD009924.pub2] [PMID: 25739460] ]. However, this review concluded that while supplementary feeding interventions can work, these interventions fail to meet the initial expectations likely due to sub-optimal implementation.
Other interventions using single- or multiple micronutrient supplementation have also aimed to improve linear and ponderal growth in young children with nutritional deficits. However, the effect of these interventions on growth is variable. In an RCT conducted in 4–36-month-old Vietnamese children with stunting and underweight status, daily zinc supplementation (10 mg/day) for 5 months significantly improved mean HAZ (0.29 unit increase from baseline) and WAZ (0.18 unit increase from baseline) compared with placebo; the change in WHZ was not significantly different between the treatment and control groups [45Ninh NX, Thissen JP, Collette L, Gerard G, Khoi HH, Ketelslegers JM. Zinc supplementation increases growth and circulating insulin-like growth factor I (IGF-I) in growth-retarded Vietnamese children. Am J Clin Nutr 1996; 63(4): 514-9.
[http://dx.doi.org/10.1093/ajcn/63.4.514] [PMID: 8599314] ]. Relative to our study, Ninh et al. reported a slightly higher HAZ increase with zinc supplementation, possibly due to the younger age of children in that study compared to that participated in our study. In contrast, other meta-analyses have found that zinc supplementation has a limited impact on growth parameters as well as stunting, underweight, and wasting status in children [46Liu E, Pimpin L, Shulkin M, et al. Effect of Zinc Supplementation on Growth Outcomes in Children under 5 Years of Age. Nutrients 2018; 10(3)E377
[http://dx.doi.org/10.3390/nu10030377] [PMID: 29558383] , 47Stammers AL, Lowe NM, Medina MW, et al. The relationship between zinc intake and growth in children aged 1-8 years: a systematic review and meta-analysis. Eur J Clin Nutr 2015; 69(2): 147-53.
[http://dx.doi.org/10.1038/ejcn.2014.204] [PMID: 25335444] ]. There is also a controversy on the efficacy of multiple micronutrient supplementation for linear growth and stunting [19Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36.
[http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] , 26Salam RA, MacPhail C, Das JK, Bhutta ZA. Effectiveness of Micronutrient Powders (MNP) in women and children. BMC Public Health 2013; 13(Suppl. 3): S22.
[PMID: 24564207] , 28Imdad A, Bhutta ZA. Effect of preventive zinc supplementation on linear growth in children under 5 years of age in developing countries: a meta-analysis of studies for input to the lives saved tool. BMC Public Health 2011; 11(Suppl. 3): S22.
[http://dx.doi.org/10.1186/1471-2458-11-S3-S22] [PMID: 21501440] , 48Ramakrishnan U, Nguyen P, Martorell R. Effects of micronutrients on growth of children under 5 y of age: meta-analyses of single and multiple nutrient interventions. Am J Clin Nutr 2009; 89(1): 191-203.
[http://dx.doi.org/10.3945/ajcn.2008.26862] [PMID: 19056559] ], with one review concluding that although multiple micronutrient interventions improve linear growth, the benefits are small [48Ramakrishnan U, Nguyen P, Martorell R. Effects of micronutrients on growth of children under 5 y of age: meta-analyses of single and multiple nutrient interventions. Am J Clin Nutr 2009; 89(1): 191-203.
[http://dx.doi.org/10.3945/ajcn.2008.26862] [PMID: 19056559] ]. Indeed, a meta-analysis in children ≥ 2 years of age who have experienced growth failure found that while single micronutrients (zinc, vitamin A), multiple micronutrients, and macronutrients (protein) significantly improve linear growth, protein supplementation had a larger effect size (mean difference [MD] 0.68) on linear growth than zinc (MD 0.15), vitamin A (MD 0.05), and multiple micronutrient sole supplementation (MD 0.26) [19Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36.
[http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] ]. In this context, multiple micronutrient interventions alone may not be sufficient to adequately overcome stunting as protein is an important macronutrient for linear growth [26Salam RA, MacPhail C, Das JK, Bhutta ZA. Effectiveness of Micronutrient Powders (MNP) in women and children. BMC Public Health 2013; 13(Suppl. 3): S22.
[PMID: 24564207] , 30Millward DJ. Nutrition, infection and stunting: the roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children. Nutr Res Rev 2017; 30(1): 50-72.
[http://dx.doi.org/10.1017/S0954422416000238] [PMID: 28112064] ]. While the extent to which our results are comparable to those from other interventions is limited by differences in the study design and populations, the ONS in our study may offer a balanced combination of energy and nutrients (micro and macro) to support catch-up growth in children with stunting [35Huynh DT, Estorninos E, Capeding RZ, Oliver JS, Low YL, Rosales FJ. Longitudinal growth and health outcomes in nutritionally at-risk children who received long-term nutritional intervention. J Hum Nutr Diet 2015; 28(6): 623-35.
[http://dx.doi.org/10.1111/jhn.12306] [PMID: 25808062] ].
In the current study, baseline HAZ and age were associated with the change in HAZ over 6 months. Children who were more severely stunted (lower HAZ) at baseline were more likely to experience improvement in HAZ during our study. This finding is consistent with another study that reported that catch-up growth in HAZ was twice as large in stunted children (aged 2–7 years) compared with marginally stunted children (−2≤ HAZ ≤ −1) [49Zhang R, Undurraga EA, Zeng W, et al. Catch-up growth and growth deficits: Nine-year annual panel child growth for native Amazonians in Bolivia. Ann Hum Biol 2016; 43(4): 304-15.
[http://dx.doi.org/10.1080/03014460.2016.1197312] [PMID: 27251215] ]. Baseline HAZ has also been shown to be a significant inverse predictor of the effect of protein and micronutrient supplementation on height in children ≥ 2 years of age [19Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36.
[http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] ]. While younger children had a greater increase in HAZ compared with older children in the present study, a meta-analysis reported that baseline age did not significantly impact the effect of nutrition interventions on height in children ≥ 2 years of age [19Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36.
[http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] ]. In addition, unlike previous studies that have demonstrated the impact of parental education on height-for-age, this factor was not significantly associated with a change in HAZ in this study [50Schott WB, Crookston BT, Lundeen EA, Stein AD, Behrman JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: key distal household and community factors. Soc Sci Med 2013; 97: 278-87.
[http://dx.doi.org/10.1016/j.socscimed.2013.05.016] [PMID: 23769211] , 51Georgiadis A, Benny L, Duc LT, Galab S, Reddy P, Woldehanna T. Growth recovery and faltering through early adolescence in low- and middle-income countries: Determinants and implications for cognitive development. Soc Sci Med 2017; 179: 81-90.
[http://dx.doi.org/10.1016/j.socscimed.2017.02.031] [PMID: 28260638] ]. This may be explained by the relative homogeneity of our study population, which was recruited from a single province in Vietnam, as well as the similar maternal education levels in our study.
Our study was conducted in children aged 24–48 months, which is beyond the ‘first 1000 days’ window. This window, from conception to 2 years of age, is widely recognized as the critical time for implementing nutritional interventions for stunting, with interventions outside this window considered unlikely to impact catch-up growth [8Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013; 382(9890): 427-51.
[http://dx.doi.org/10.1016/S0140-6736(13)60937-X] [PMID: 23746772] , 52Victora CG, de Onis M, Hallal PC, Blössner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 2010; 125(3): e473-80.
[http://dx.doi.org/10.1542/peds.2009-1519] [PMID: 20156903] ]. However, several longitudinal studies have demonstrated that catch-up linear growth still occurs after the ‘first 1000 days’ [53Lundeen EA, Behrman JR, Crookston BT, et al. Growth faltering and recovery in children aged 1-8 years in four low- and middle-income countries: Young Lives. Public Health Nutr 2014; 17(9): 2131-7.
[http://dx.doi.org/10.1017/S1368980013003017] [PMID: 24477079] , 54Prentice AM, Ward KA, Goldberg GR, et al. Critical windows for nutritional interventions against stunting. Am J Clin Nutr 2013; 97(5): 911-8.
[http://dx.doi.org/10.3945/ajcn.112.052332] [PMID: 23553163] ]. The Young Lives study, a 15-year longitudinal cohort study of childhood poverty in four low and middle-income countries in Ethiopia, India, Peru, and Vietnam, found that the incidence of recovery from stunting between ages 1 and 5 years ranges from 27% (Vietnam) to 53% (Ethiopia); between ages 5 and 8 years, it ranged from 30% (India) to 47% (Ethiopia). The results suggest that catch-up from stunting post-infancy is possible and nutritional interventions to improve stunting status should also be provided to stunted children after infancy and early childhood [53Lundeen EA, Behrman JR, Crookston BT, et al. Growth faltering and recovery in children aged 1-8 years in four low- and middle-income countries: Young Lives. Public Health Nutr 2014; 17(9): 2131-7.
[http://dx.doi.org/10.1017/S1368980013003017] [PMID: 24477079] ]. Furthermore, nutrition interventions using protein, single, or multiple micronutrients have been found to positively affect linear growth after 2 years of age [19Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36.
[http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] ]. Additionally, analyses of absolute height-for-age differences indicate that linear growth deficits accumulate beyond 2 years of age, as 70% of the absolute height deficit at 60 months can be attributed to faltering during the ‘first 1000 days’ whereas 30% is due to continued increases in the deficit from age 2–5 years [55Leroy JL, Ruel M, Habicht JP, Frongillo EA. Linear growth deficit continues to accumulate beyond the first 1000 days in low- and middle-income countries: global evidence from 51 national surveys. J Nutr 2014; 144(9): 1460-6.
[http://dx.doi.org/10.3945/jn.114.191981] [PMID: 24944283] ]. In this context, our study suggests that nutritional intervention in stunted children older than 2 years is effective in promoting catch-up linear growth, which could potentially mitigate the adverse consequences of stunting. As even mild undernutrition is associated with increased mortality in children under 5 years of age, early intervention has been recommended as a preventive approach to mitigate nutrition deficits in children at risk of undernutrition [9Olofin I, McDonald CM, Ezzati M, et al. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS One 2013; 8(5)e64636
[http://dx.doi.org/10.1371/journal.pone.0064636] [PMID: 23734210] , 23de Pee S, Bloem MW. Current and potential role of specially formulated foods and food supplements for preventing malnutrition among 6- to 23-month-old children and for treating moderate malnutrition among 6- to 59-month-old children. Food Nutr Bull 2009; 30(3)(Suppl.): S434-63.
[http://dx.doi.org/10.1177/15648265090303S305] [PMID: 19998866] , 56Ruel MT, Menon P, Habicht JP, et al. Age-based preventive targeting of food assistance and behaviour change and communication for reduction of childhood undernutrition in Haiti: a cluster randomised trial. Lancet 2008; 371(9612): 588-95.
[http://dx.doi.org/10.1016/S0140-6736(08)60271-8] [PMID: 18280329] ].
Our study had some limitations. This was a single-arm clinical trial with no control group; as such, the causal effects of the ONS intervention on growth parameters need to be further established in a placebo-controlled RCT. However, considering the well-established association between poor nutrition and impaired growth in children [57Williams AM, Suchdev PS. Assessing and Improving Childhood Nutrition and Growth Globally. Pediatr Clin North Am 2017; 64(4): 755-68.
[http://dx.doi.org/10.1016/j.pcl.2017.03.001] [PMID: 28734508] ] as well as previous RCTs demonstrating the positive effect of ONS for growth [34Alarcon PA, Lin LH, Noche M Jr, et al. Effect of oral supplementation on catch-up growth in picky eaters. Clin Pediatr (Phila) 2003; 42(3): 209-17.
[http://dx.doi.org/10.1177/000992280304200304] [PMID: 12739919] , 40Ghosh AK, Kishore B, Shaikh I, et al. Effect of oral nutritional supplementation on growth and recurrent upper respiratory tract infections in picky eating children at nutritional risk: a randomized, controlled trial. J Int Med Res 2018; 46(6): 2186-201.
[http://dx.doi.org/10.1177/0300060518757355] [PMID: 29614897] ], there is a high probability that the ONS contributed to improved growth in the current study. Another limitation is the lack of assessment of dietary intake as well as parental height as a proxy for genetic influences in the analysis of the factors associated with a change in HAZ over the follow-up period.
While the long-term effects of ONS on physical growth have been established in children at nutritional risk [35Huynh DT, Estorninos E, Capeding RZ, Oliver JS, Low YL, Rosales FJ. Longitudinal growth and health outcomes in nutritionally at-risk children who received long-term nutritional intervention. J Hum Nutr Diet 2015; 28(6): 623-35.
[http://dx.doi.org/10.1111/jhn.12306] [PMID: 25808062] ], further studies evaluating the long-term impact of ONS on height and weight in children with stunting are warranted. Additionally, as overcoming chronic undernutrition requires an integrated approach, studies examining the efficacy of combining diet and supplementation for stunting could provide useful insights. In developing countries, assessing the cost-effectiveness of nutritional interventions in children with stunting is likely to have important public health implications.
CONCLUSION
In conclusion, nutritional intervention with ONS appears to be beneficial for improving physical growth in stunted children at risk of wasting. Furthermore, the energy, macronutrients and micronutrients provided by this intervention have the potential to reduce stunting, underweight and wasting status in stunted children.
LIST OF ABBREVIATIONS
| AEs | = Adverse Events; |
| DC | = Dietary Counseling; |
| HAZ | = Height-for-Age z-Score; |
| IQR | = Interquartile Range; |
| LNS | = Lipid-based Nutrient Supplements; |
| ONS | = Oral Nutritional Supplementation; |
| RCT | = Randomized Controlled Trial; |
| SD | = Standard Deviation; |
| WAZ | = Weight-for-Age z-Score; |
| WHZ | = Weight-for-Height z-Score; |
| WHO | = World Health Organization. |
AUTHORS’ CONTRIBUTIONS
DTP, TNH, NTN, LHN, TQT and NTN conceived and designed the study. DTP, TNH, NTN, LHN, TQT and NTN were responsible for subject recruitment and data collection. DTP, HMP, DTTH and NTN participated in data analysis and interpretation. DTP, DTTH and NTN contributed to manuscript drafting. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by Institutional Review Board of the Thai Binh University of Medicine and Pharmacy and the reference number of ethical committee is 5/2016.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from each child’s parents or legal guardian prior to the study initiation.
AVAILABILITY OF DATA & MATERIAL
The data that support the findings of this study are available from the corresponding author, [Dung T. Pham], upon reasonable request.
FUNDING
This study was funded by Thai Binh University of Medicine and Pharmacy. The funding agency reference number is 1596. It was partially supported by Abbott Nutrition.
CONFLICT OF INTEREST
The study was partially supported by Abbott Nutrition. DTTH is an employee of Abbott Nutrition.
ACKNOWLEDGEMENTS
We are grateful to children and their parents who participated in this study. We gratefully acknowledge the assistance of school teachers for study execution. Editorial assistance for this manuscript was provided by Aishwarya Sridharan from in vivo Communications (Asia).
REFERENCES
| [1] | UNICEF, WHO, World Bank Group. Levels and trends in child malnutrition 2018.https://www.who.int/nutgrowthdb/2018-jme-brochure.pdf?ua=1 |
| [2] | WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 2006; 450(Suppl. 450): 76-85. [PMID: 16817681] |
| [3] | Report GN. Global Nutrition Report. 2017 Global Nutrition Report. 2017 [cited 2018 Dec 13]. Available from: https://globalnutritionreport .org/reports/2017-global-nutrition-report/ |
| [4] | Food and Agriculture Organization of the United Nations. Viet Nam - Food and Nutrition Security Profiles. 2014 [accessed 13 December 2018]. Available from: http://www.fao.org/3/a-at704e.pdf. |
| [5] | Chaparro C, Oot L, Sethuraman K. Vietnam Nutrition Profile 2014.https://www.fantaproject.org/sites/default/files/download/Vietnam-Nutrition-Profile-Apr2014.pdf |
| [6] | Ali D, Saha KK, Nguyen PH, et al. Household food insecurity is associated with higher child undernutrition in Bangladesh, Ethiopia, and Vietnam, but the effect is not mediated by child dietary diversity. J Nutr 2013; 143(12): 2015-21. [http://dx.doi.org/10.3945/jn.113.175182] [PMID: 24089419] |
| [7] | Nguyen PH, Menon P, Ruel M, Hajeebhoy N. A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pac J Clin Nutr 2011; 20(3): 359-74. [PMID: 21859654] |
| [8] | Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013; 382(9890): 427-51. [http://dx.doi.org/10.1016/S0140-6736(13)60937-X] [PMID: 23746772] |
| [9] | Olofin I, McDonald CM, Ezzati M, et al. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies. PLoS One 2013; 8(5)e64636 [http://dx.doi.org/10.1371/journal.pone.0064636] [PMID: 23734210] |
| [10] | Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet 2007; 369(9555): 60-70. [http://dx.doi.org/10.1016/S0140-6736(07)60032-4] [PMID: 17208643] |
| [11] | Prendergast AJ, Humphrey JH. The stunting syndrome in developing countries. Paediatr Int Child Health 2014; 34(4): 250-65. [http://dx.doi.org/10.1179/2046905514Y.0000000158] [PMID: 25310000] |
| [12] | Walker SP, Chang SM, Powell CA, Simonoff E, Grantham-McGregor SM. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation. J Nutr 2007; 137(11): 2464-9. [http://dx.doi.org/10.1093/jn/137.11.2464] [PMID: 17951486] |
| [13] | Adair LS, Fall CH, Osmond C, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet 2013; 382(9891): 525-34. [http://dx.doi.org/10.1016/S0140-6736(13)60103-8] [PMID: 23541370] |
| [14] | Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008; 371(9609): 340-57. [http://dx.doi.org/10.1016/S0140-6736(07)61692-4] [PMID: 18206223] |
| [15] | Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S. The economic rationale for investing in stunting reduction. Matern Child Nutr 2013; 9(Suppl. 2): 69-82. [http://dx.doi.org/10.1111/mcn.12080] [PMID: 24074319] |
| [16] | Martorell R, Horta BL, Adair LS, et al. Weight gain in the first two years of life is an important predictor of schooling outcomes in pooled analyses from five birth cohorts from low- and middle-income countries. J Nutr 2010; 140(2): 348-54. [http://dx.doi.org/10.3945/jn.109.112300] [PMID: 20007336] |
| [17] | Golden MH. Proposed recommended nutrient densities for moderately malnourished children. Food Nutr Bull 2009; 30(3)(Suppl.): S267-342. [http://dx.doi.org/10.1177/15648265090303S302] [PMID: 19998863] |
| [18] | Michaelsen KF, Hoppe C, Roos N, et al. Choice of foods and ingredients for moderately malnourished children 6 months to 5 years of age. Food Nutr Bull 2009; 30(3)(Suppl.): S343-404. [http://dx.doi.org/10.1177/15648265090303S303] [PMID: 19998864] |
| [19] | Roberts JL, Stein AD. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv Nutr 2017; 8(2): 323-36. [http://dx.doi.org/10.3945/an.116.013938] [PMID: 28298275] |
| [20] | Marriott BP, White A, Hadden L, Davies JC, Wallingford JC. World Health Organization (WHO) infant and young child feeding indicators: associations with growth measures in 14 low-income countries. Matern Child Nutr 2012; 8(3): 354-70. [http://dx.doi.org/10.1111/j.1740-8709.2011.00380.x] [PMID: 22171937] |
| [21] | Ashworth A, Ferguson E. Dietary counseling in the management of moderate malnourishment in children. Food Nutr Bull 2009; 30(3)(Suppl.): S405-33. [http://dx.doi.org/10.1177/15648265090303S304] [PMID: 19998865] |
| [22] | Bhutta ZA, Ahmed T, Black RE, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet 2008; 371(9610): 417-40. [http://dx.doi.org/10.1016/S0140-6736(07)61693-6] [PMID: 18206226] |
| [23] | de Pee S, Bloem MW. Current and potential role of specially formulated foods and food supplements for preventing malnutrition among 6- to 23-month-old children and for treating moderate malnutrition among 6- to 59-month-old children. Food Nutr Bull 2009; 30(3)(Suppl.): S434-63. [http://dx.doi.org/10.1177/15648265090303S305] [PMID: 19998866] |
| [24] | Pham VP, Nguyen VH, Salvignol B, et al. A six-month intervention with two different types of micronutrient-fortified complementary foods had distinct short- and long-term effects on linear and ponderal growth of Vietnamese infants. J Nutr 2012; 142(9): 1735-40. [http://dx.doi.org/10.3945/jn.111.154211] [PMID: 22810985] |
| [25] | Fleige LE, Moore WR, Garlick PJ, et al. Recommendations for optimization of fortified and blended food aid products from the United States. Nutr Rev 2010; 68(5): 290-315. [http://dx.doi.org/10.1111/j.1753-4887.2010.00288.x] [PMID: 20500790] |
| [26] | Salam RA, MacPhail C, Das JK, Bhutta ZA. Effectiveness of Micronutrient Powders (MNP) in women and children. BMC Public Health 2013; 13(Suppl. 3): S22. [PMID: 24564207] |
| [27] | Allen LH, Peerson JM, Olney DK. Provision of multiple rather than two or fewer micronutrients more effectively improves growth and other outcomes in micronutrient-deficient children and adults. J Nutr 2009; 139(5): 1022-30. [http://dx.doi.org/10.3945/jn.107.086199] [PMID: 19321586] |
| [28] | Imdad A, Bhutta ZA. Effect of preventive zinc supplementation on linear growth in children under 5 years of age in developing countries: a meta-analysis of studies for input to the lives saved tool. BMC Public Health 2011; 11(Suppl. 3): S22. [http://dx.doi.org/10.1186/1471-2458-11-S3-S22] [PMID: 21501440] |
| [29] | De-Regil LM, Suchdev PS, Vist GE, Walleser S, Peña-Rosas JP. Home fortification of foods with multiple micronutrient powders for health and nutrition in children under two years of age. Cochrane Database Syst Rev 2011; 9(9)CD008959 [http://dx.doi.org/10.1002/14651858.CD008959.pub2] [PMID: 21901727] |
| [30] | Millward DJ. Nutrition, infection and stunting: the roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children. Nutr Res Rev 2017; 30(1): 50-72. [http://dx.doi.org/10.1017/S0954422416000238] [PMID: 28112064] |
| [31] | Maleta KM, Phuka J, Alho L, et al. Provision of 10-40 g/d Lipid-Based Nutrient Supplements from 6 to 18 Months of Age Does Not Prevent Linear Growth Faltering in Malawi. J Nutr 2015; 145(8): 1909-15. [http://dx.doi.org/10.3945/jn.114.208181] [PMID: 26063066] |
| [32] | Style S, Tondeur M, Grijalva-Eternod C, et al. Assessment of the effectiveness of a small quantity lipid-based nutrient supplement on reducing anaemia and stunting in refugee populations in the Horn of Africa: Secondary data analysis. PLoS One 2017; 12(6)e0177556 [http://dx.doi.org/10.1371/journal.pone.0177556] [PMID: 28591166] |
| [33] | Adu-Afarwuah S, Lartey A, Okronipa H, et al. Small-quantity, lipid-based nutrient supplements provided to women during pregnancy and 6 mo postpartum and to their infants from 6 mo of age increase the mean attained length of 18-mo-old children in semi-urban Ghana: a randomized controlled trial. Am J Clin Nutr 2016; 104(3): 797-808. [http://dx.doi.org/10.3945/ajcn.116.134692] [PMID: 27534634] |
| [34] | Alarcon PA, Lin LH, Noche M Jr, et al. Effect of oral supplementation on catch-up growth in picky eaters. Clin Pediatr (Phila) 2003; 42(3): 209-17. [http://dx.doi.org/10.1177/000992280304200304] [PMID: 12739919] |
| [35] | Huynh DT, Estorninos E, Capeding RZ, Oliver JS, Low YL, Rosales FJ. Longitudinal growth and health outcomes in nutritionally at-risk children who received long-term nutritional intervention. J Hum Nutr Diet 2015; 28(6): 623-35. [http://dx.doi.org/10.1111/jhn.12306] [PMID: 25808062] |
| [36] | Huynh DT, Estorninos E, Capeding MR, Oliver JS, Low YL, Rosales FJ. Impact of long-term use of oral nutritional supplement on nutritional adequacy, dietary diversity, food intake and growth of Filipino preschool children. J Nutr Sci 2016; 5: e20. [http://dx.doi.org/10.1017/jns.2016.6] [PMID: 27293557] |
| [37] | Lebenthal Y, Yackobovitch-Gavan M, Lazar L, et al. Effect of a nutritional supplement on growth in short and lean prepubertal children: a prospective, randomized, double-blind, placebo-controlled study. J Pediatr 2014; 165(6): 1190-1193.e1. [http://dx.doi.org/10.1016/j.jpeds.2014.08.011] [PMID: 25241181] |
| [38] | Bhutta Z, Yackobovitch-Gavan M. Malnutrition and Catch-Up Growth during Childhood and Puberty. World Rev Nutr Diet 2016; 114: 120-7. [http://dx.doi.org/10.1159/000441823] [PMID: 26914906] |
| [39] | Sheng X, Tong M, Zhao D, et al. Randomized controlled trial to compare growth parameters and nutrient adequacy in children with picky eating behaviors who received nutritional counseling with or without an oral nutritional supplement. Nutr Metab Insights 2014; 7: 85-94. [http://dx.doi.org/10.4137/NMI.S15097] [PMID: 25342910] |
| [40] | Ghosh AK, Kishore B, Shaikh I, et al. Effect of oral nutritional supplementation on growth and recurrent upper respiratory tract infections in picky eating children at nutritional risk: a randomized, controlled trial. J Int Med Res 2018; 46(6): 2186-201. [http://dx.doi.org/10.1177/0300060518757355] [PMID: 29614897] |
| [41] | Sazawal S, Dhingra U, Dhingra P, et al. Micronutrient fortified milk improves iron status, anemia and growth among children 1-4 years: a double masked, randomized, controlled trial. PLoS One 2010; 5(8): e12167. [http://dx.doi.org/10.1371/journal.pone.0012167] [PMID: 20730057] |
| [42] | Tran TQ. Prevalence of stunting and the effects of consumption of a locally available seafood in improving stunting in children under 5 years old in Tien Hai, a coastal area of Thai Binh province, Vietnam. Thai Binh University of Medicine and Pharmacy, Vietnam 2014 Unpublished study |
| [43] | Nguyen VA, Le HT, Pham HTT, Doan HTT. Effect of supplementary feeding using locally available foods on improving stunting, Tien Lu district, Hung Yen Province. Vietnam Journal of Practical Medicine 2017; 1033: 35-9. |
| [44] | Kristjansson E, Francis DK, Liberato S, et al. Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years. Cochrane Database Syst Rev 2015; 3(3): CD009924. [http://dx.doi.org/10.1002/14651858.CD009924.pub2] [PMID: 25739460] |
| [45] | Ninh NX, Thissen JP, Collette L, Gerard G, Khoi HH, Ketelslegers JM. Zinc supplementation increases growth and circulating insulin-like growth factor I (IGF-I) in growth-retarded Vietnamese children. Am J Clin Nutr 1996; 63(4): 514-9. [http://dx.doi.org/10.1093/ajcn/63.4.514] [PMID: 8599314] |
| [46] | Liu E, Pimpin L, Shulkin M, et al. Effect of Zinc Supplementation on Growth Outcomes in Children under 5 Years of Age. Nutrients 2018; 10(3)E377 [http://dx.doi.org/10.3390/nu10030377] [PMID: 29558383] |
| [47] | Stammers AL, Lowe NM, Medina MW, et al. The relationship between zinc intake and growth in children aged 1-8 years: a systematic review and meta-analysis. Eur J Clin Nutr 2015; 69(2): 147-53. [http://dx.doi.org/10.1038/ejcn.2014.204] [PMID: 25335444] |
| [48] | Ramakrishnan U, Nguyen P, Martorell R. Effects of micronutrients on growth of children under 5 y of age: meta-analyses of single and multiple nutrient interventions. Am J Clin Nutr 2009; 89(1): 191-203. [http://dx.doi.org/10.3945/ajcn.2008.26862] [PMID: 19056559] |
| [49] | Zhang R, Undurraga EA, Zeng W, et al. Catch-up growth and growth deficits: Nine-year annual panel child growth for native Amazonians in Bolivia. Ann Hum Biol 2016; 43(4): 304-15. [http://dx.doi.org/10.1080/03014460.2016.1197312] [PMID: 27251215] |
| [50] | Schott WB, Crookston BT, Lundeen EA, Stein AD, Behrman JR. Periods of child growth up to age 8 years in Ethiopia, India, Peru and Vietnam: key distal household and community factors. Soc Sci Med 2013; 97: 278-87. [http://dx.doi.org/10.1016/j.socscimed.2013.05.016] [PMID: 23769211] |
| [51] | Georgiadis A, Benny L, Duc LT, Galab S, Reddy P, Woldehanna T. Growth recovery and faltering through early adolescence in low- and middle-income countries: Determinants and implications for cognitive development. Soc Sci Med 2017; 179: 81-90. [http://dx.doi.org/10.1016/j.socscimed.2017.02.031] [PMID: 28260638] |
| [52] | Victora CG, de Onis M, Hallal PC, Blössner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 2010; 125(3): e473-80. [http://dx.doi.org/10.1542/peds.2009-1519] [PMID: 20156903] |
| [53] | Lundeen EA, Behrman JR, Crookston BT, et al. Growth faltering and recovery in children aged 1-8 years in four low- and middle-income countries: Young Lives. Public Health Nutr 2014; 17(9): 2131-7. [http://dx.doi.org/10.1017/S1368980013003017] [PMID: 24477079] |
| [54] | Prentice AM, Ward KA, Goldberg GR, et al. Critical windows for nutritional interventions against stunting. Am J Clin Nutr 2013; 97(5): 911-8. [http://dx.doi.org/10.3945/ajcn.112.052332] [PMID: 23553163] |
| [55] | Leroy JL, Ruel M, Habicht JP, Frongillo EA. Linear growth deficit continues to accumulate beyond the first 1000 days in low- and middle-income countries: global evidence from 51 national surveys. J Nutr 2014; 144(9): 1460-6. [http://dx.doi.org/10.3945/jn.114.191981] [PMID: 24944283] |
| [56] | Ruel MT, Menon P, Habicht JP, et al. Age-based preventive targeting of food assistance and behaviour change and communication for reduction of childhood undernutrition in Haiti: a cluster randomised trial. Lancet 2008; 371(9612): 588-95. [http://dx.doi.org/10.1016/S0140-6736(08)60271-8] [PMID: 18280329] |
| [57] | Williams AM, Suchdev PS. Assessing and Improving Childhood Nutrition and Growth Globally. Pediatr Clin North Am 2017; 64(4): 755-68. [http://dx.doi.org/10.1016/j.pcl.2017.03.001] [PMID: 28734508] |